Medical term:
FiberNorm
calcium
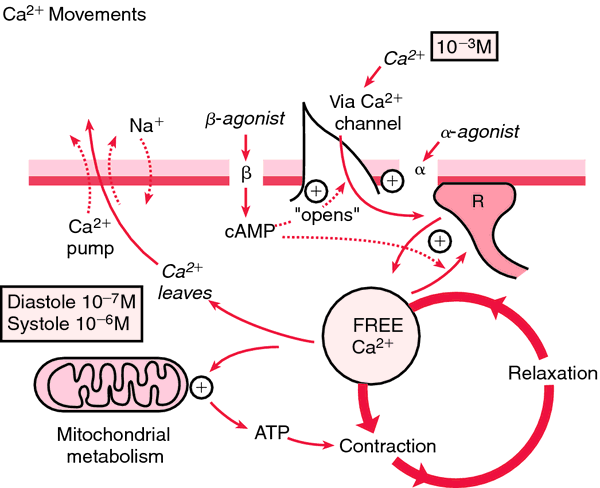
(Ca) [kal´se-um]Within the body fluids calcium exists in three forms. Protein-bound calcium accounts for about 47 per cent of the calcium in plasma; most of it in this form is bound to albumin. Another 47 per cent of plasma calcium is ionized. About 6 per cent is complexed with phosphate, citrate, and other anions.
Ionized calcium is physiologically active. One of its most important physiological functions is control of the permeability of cell membranes. Parathyroid hormone, which causes transfer of exchangeable calcium from bone into the blood stream, maintains calcium homeostasis by preventing either calcium deficit or excess.
Hypercalcemia: This is when the level of serum calcium rises above normal; neuromuscular activity begins to diminish. Symptoms include lethargy, muscle weakness (which, as the level of calcium increases, can progress to depressed reflexes and hypotonic muscles), constipation, mental confusion, and coma. The heartbeat also slows, which potentiates the effects of digitalis.
Hypocalcemia: This is a serum level of calcium that is below normal; it is manifested by increased neuromuscular irritability. When there is a deficit of ionized calcium, the nerve cells become more permeable, allowing leakage of sodium and potassium from the cells. This produces excitation of the nerve fibers and triggers uncontrollable activity of the skeletal muscles. Hence, as the calcium level continues to drop, the patient begins to experience muscle twitching and cramping, grimacing, and carpopedal spasm, which can quickly progress to tetany, laryngospasm, convulsions, cardiac arrhythmias, and eventually to respiratory and cardiac arrest. Relatively early signs of hypocalcemia are a positive trousseau's sign and a positive chvostek's sign.
Dietary sources of calcium include dairy products (such as milk and cheese), soybeans, fortified orange juice, dark green leafy vegetables (such as mustard greens and broccoli), sardines, clams, and oysters. The recommended dietary allowance of calcium for children aged 4 to 8 is 800 mg, and that for women aged 50 to 70 is 1200 mg. (See tables in the Appendices for recommended dietary allowances across the life span.) It is difficult to meet these requirements without including milk or milk products in the daily diet. The most familiar calcium deficiency disease is rickets, in which the bones and teeth soften. However, it is believed that a large number of people suffer from subclinical calcium deficiency because of poor eating habits. Since calcium is essential to the formation and maintenance of strong bones, an adequate intake is important in the prevention of osteoporosis.
calcium polycarbophil
Pharmacologic class: Bulk-forming agent
Therapeutic class: Laxative
Pregnancy risk category NR
Action
Absorbs water, thereby expanding and increasing bulk and moisture content of stool; increased bulk promotes peristalsis and bowel movement.
Availability
Tablets: 500 mg
Tablets (chewable): 500 mg, 1,250 mg
Indications and dosages
➣ Constipation
Adults and children ages 12 and older: 1 g P.O. q.i.d. as needed. Maximum dosage is 6 g daily.
Children ages 7 to 12: 500 mg P.O. one to three times daily as needed. Maximum dosage is 3 g daily.
Children ages 3 to 6: 500 mg P.O. b.i.d. as needed. Maximum dosage is 1.5 g daily.
➣ Diarrhea; irritable bowel syndrome
Adults and children ages 12 and older: 1 g P.O. q.i.d. as needed. Maximum dosage is 6 g daily.
Children ages 7 to 12: 500 mg P.O. one to three times daily as needed. Maximum dosage is 3 g in a 24-hour period.
Children ages 3 to 6: 500 mg P.O. b.i.d. as needed. Maximum dosage is 1.5 g daily.
Contraindications
• GI obstruction
• Difficulty swallowing
Precautions
Use cautiously in:
• pregnant or breastfeeding patients
• children.
Administration
• Give with at least 8 oz of water or other fluid.
• Administer at least 2 hours before or after other drugs.
• Make sure patient maintains adequate fluid intake.
Adverse reactions
CV: chest pain
GI: nausea, vomiting, abdominal pain, flatulence, rectal bleeding, intestinal obstruction
Respiratory: difficulty breathing
Other: laxative dependence
Interactions
Drug-drug. Tetracyclines: impaired tetracycline absorption
Drug-herbs. Lily of the valley, pheasant's eye, squill: increased risk of adverse drug reactions
Patient monitoring
☞ Monitor patient for difficulty breathing and signs and symptoms of intestinal obstruction.
• Assess for rectal bleeding and for failure to respond to drug.
• Monitor fluid intake and output, and assess hydration status regularly.
Patient teaching
• Instruct patient to take each dose with at least 8 oz of water or other fluid.
• Advise patient to space doses at least 2 hours apart from other drugs.
☞ Urge patient to seek immediate medical attention if he experiences chest pain, vomiting, difficulty breathing, or rectal bleeding.
• Advise patient to tell prescriber if he's taking other drugs or if he has abdominal pain, nausea, vomiting, or a sudden change in bowel habits lasting 2 weeks or longer.
• As appropriate, review all other significant and life-threatening adverse reactions and interactions, especially those related to the drugs and herbs mentioned above.
Latest Searches:
ZPLATE - Zovia - Zovant - Zouchlos' - Zoto - Zosyn - Zostrix - zostervirus - zosteroid - zosteriform - zoster - zorubicin - Zortress - ZORprin - Zorbtive - zorbamycin - Zorac - zopolrestat - zopiclone - Zopfius -
- Service manuals - MBI Corp