Medical term:
Hysterectomy
Hysterectomy
Definition
Purpose
Alternatives
Embolization
Myomectomy
Endometrial ablation
Endometrial resection
Total hysterectomy
Subtotal hysterectomy
Radical hysterectomy
Precautions

Description
Abdominal hysterectomy
Vaginal hysterectomy
Preparation
Aftercare
Risks
Normal results
Key terms
Resources
Organizations
Other
hysterectomy
[his″tĕ-rek´to-me]Incisions made above and around the cervix in vaginal hysterectomy heal more rapidly than do abdominal incisions, and intestinal complications such as ileus are less likely. However, vaginal hysterectomy patients have a higher incidence of postoperative bleeding and infections, especially of the urinary tract.
There should be sufficient time to determine what the patient knows, to answer her questions, and to dispel any misinformation she might have. Preoperative teaching does not necessarily mean that it is done the night before surgery. In fact, at that time the patient may be preoccupied with anxieties about major surgery and fears about pain and perhaps death. In that state of mind she would probably be unable to assimilate most factual information presented to her. At this point relieving the patient's anxiety is a top priority.
A patient's ability to adjust to the loss of a reproductive organ will be influenced by her sense of self as a woman, her age and previous socialization in regard to the roles of women, and the attitudes and expectations of her spouse, family and friends. Negative or positive attitudes can arise from her beliefs about how the surgery will affect her sexual expression and function and her vocational and avocational involvement and enjoyment of life. If the woman has experienced long-term pain and discomfort or has no desire to have more children, she may be favorably disposed toward the surgery. However, she may feel a profound sense of loss and purpose in her life. Negative attitudes toward the hysterectomy can have serious and adverse psychologic effects months or even years after the surgery.
Bleeding is a potential danger because of the abundant vascularity of the female pelvis. Dressings and perineal pads are checked regularly every two to four hours, or more often as indicated. The patient who has had vaginal surgery usually has a vaginal packing with a drain attached to the distal end. Some vaginal bleeding and oozing of serosanguineous fluid can be expected, but if there is frank bleeding of more than a light menstrual flow, or if the patient is passing clots around the pack, there is cause for concern. Heavy bleeding, a rapidly distended abdomen, referred shoulder pain, and change in vital signs are signs of an emergency that requires a return to the operating room to find and stop the source of blood loss.
Patients with an abdominal incision are monitored and dressings checked for excessive bleeding. If there is evidence of increasingly larger deposits of blood on the dressing, reinforcement of the dressing and notification of the surgeon are indicated.
The urinary output and characteristics of the urine are observed for signs of urinary tract infection. If the patient has an indwelling catheter, special catheter care is necessary. A poorly draining catheter or one that is totally blocked can lead to bladder distention and abdominal pressure. To avoid additional pressure on the abdomen and sutures, the patient is positioned on her side or back with her knees slightly flexed. High Fowler's position is contraindicated and there should be no pillows or break in the bed to produce pressure behind the knees.
Prior to discharge from the hospital the patient is given instructions in self-care; these should be written so that the patient can refer to them at home if necessary. They should include information about surgical menopause and estrogen therapy if the ovaries were removed; restrictions on douching and sexual intercourse; prevention of constipation; care of the incision; and reportable symptoms such as redness, swelling, pain, or drainage at the operative site and elevation of body temperature. Abdominal cramps and changes in bowel habits also should be reported to the professional caregiver.
The patient should also have opportunities to discuss personal contacts regarding sexual activity and her new body image. Although this may have been discussed during the preoperative period, she may be more receptive after the surgery is over and she is on the way to recovery. Some hospitals and clinics have support groups for women contemplating or recovering from hysterectomy. These can be a great support to patients and provide them with additional information and a forum for expressing and dealing with their emotional reactions to hysterectomy.
hys·ter·ec·to·my
(his'ter-ek'tŏ-mē),hysterectomy
(hĭs′tə-rĕk′tə-mē)hysterectomy
Gynecology The 2nd most common–after C sections–operation performed in the US ± 590,000/yr, ±4/1000 ♀/yr; annual cost ± $5 x 109; in developed nations, there is a 6-fold range in frequency of hysterectomy–highest in US, lowest in Sweden, Norway, UK Indications Uterine leiomyomas–30%, dysfunctional uterine bleeding–20%, endometriosis and adenomyosis–20%, genital prolapse–15%, chronic pelvic pain–10%, PID, endometrial hyperplasia, and other malignancy–eg, CIN, endometrial CA, and other indications–eg, massive postpartum hemorrhage, septic endometritis, hormone therapy where estrogen receptors are positive Procedures Total abdominal, total vaginal, laparoscopic vaginal Complications Fever, infection, intra- and post-operative hemorrhage, urinary Sx, early ovary failure, retained ovary syndrome, constipation, fatigue, ↓ sexual interest and function, depression, psychiatric morbidity Mortality 7-20 deaths/105 hysterectomies for cancer, 3-4 deaths/105 for pregnancy-related indications, 0.6-1.1 deaths/105 hysterectomies for other indications Sexology ↑ Frequency, orgasms, sexual desire, ↓ dyspareunia posthysterectomy. See Abdominal hysterectomy, Complete hysterectomy, TAH-BSO, Total abdominal hysterectomy, Vaginal hysterectomy. Cf Laparoscopic vaginal hysterectomy.hys·ter·ec·to·my
(his'tĕr-ek'tŏ-mē)hysterectomy
(his?te-rek'to-me) [ hystero- + -ectomy]

In preparation for abdominal hysterectomy, the patient is placed in the dorsal position. The table is ready to be tipped into the Trendelenburg position. As soon as the incision is made through the peritoneum, the table should be put into the Trendelenburg position. This procedure is the same for all abdominopelvic surgery, as the Trendelenburg position allows the abdominal organs to fall away from the pelvis so that they may be easily packed off and isolated from the surgical field with large pads or a large roll of packing.
Patient care
Preoperative: In general, preparations for an abdominal hysterectomy are similar to protocols for any abdominopelvic surgery (e.g., abdominal skin preparation, insertion of an intravenous line and, depending on surgical protocol, an indwelling urinary catheter). Vaginal irrigation with antibacterial solution also may be ordered. All procedures are explained to the patient, who is provided with anticipatory guidance for the postoperative period. Misconceptions are clarified, informed consent is validated, and the signing of the operative permit is witnessed. The patient may be encouraged to discuss the personal meaning and implications of the procedure, such as permanent inability to bear children; emotional support is given. The gynecologist and nurses should make available opportunities for the patient to ask questions and receive information about sexual concerns and be provided with resources (or a way to access resources), or specialist referrals for further information as desired. Controlled trials that have studied large numbers of women have not shown, in aggregate, any adverse effect of hysterectomy on sexuality (good sexual function is retained or regained; however the nature and quality of sexual response may change) or women's perceptions of their femininity.
Postoperative: Initial status assessments include color; vital signs; airway patency and breath sounds; level of consciousness and discomfort; intravenous intake; and nasogastric and indwelling catheter drainage. During the first few hours, assessments usually are made over lengthening intervals, from every 10 to 15 minutes during the first hour to every 30 minutes to hourly. Intervals and assessment priorities may be altered on the basis of current findings, such as bleeding. Color; vital signs; airway patency and lung sounds; level of consciousness and discomfort; intake and output (including intravenous fluids, nasogastric and indwelling catheter drainage); and abdominal dressings (intact, amount and character of any drainage) are monitored. Additional later assessments include bowel sounds; lower extremity circulation (pedal pulses, leg pain); and wound status (redness, edema, ecchymosis, discharge, and approximation). The patient is encouraged to splint the incision, turn from side to side, use incentive spirometry, deep breathe and cough every 2 hr, and use incentive spirometry. Prescribed intravenous fluids and analgesics are administered. The woman is assisted in self-administering patient-controlled analgesia. Antithromboembolitic devices (pneumatic dressings or elastic stockings) are applied as needed. The patient is encouraged and assisted with early ambulation. The patient is encouraged to splint the incision, turn from side to side, deep breathe and cough every 2 hr, and use incentive spirometry.
If the patient's ovaries have been removed, the reasons for hormone therapy are explained to her. Effective coping strategies related to anticipated radiation and/or chemotherapy are targeted. Desired outcomes include evidence of incisional healing; absence of complications; return of normal GI and bladder function; and understanding of and compliance with the prescribed treatment regimen.
abdominal hysterectomy
cesarean hysterectomy
pan hysterectomy
radical hysterectomy
subtotal hysterectomy
supracervical hysterectomy
Subtotal hysterectomy.supravaginal hysterectomy
Subtotal hysterectomy.total abdominal hysterectomy
vaginal hysterectomy
hysterectomy
Surgical removal of the womb (uterus). This may be done through the vagina (vaginal hysterectomy) or through an incision in the abdominal wall (abdominal hysterectomy). The operation is performed to treat extensive FIBROIDS, cancer of the womb, ENDOMETRIOSIS, excessive menstruation (MENORRHAGIA), for purposes of sterilization or out of fear of possible later womb cancer. In some affluent countries hysterectomy is grossly over-performed. In California, for instance, almost half of all women undergo hysterectomy.Patient discussion about hysterectomy
Q. What Is a Hysterectomy? I am 60 year old. My doctor told me I night need to undergo a hysterectomy because I have large fibroids, that most likely not malignant, however they do cause bleeding. What exactly is a hysterectomy?
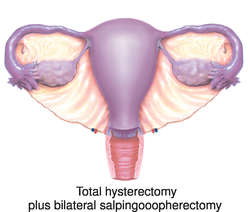
*Complete or total. Removes the cervix as well as the uterus. (This is the most common type of hysterectomy.)
*Partial or subtotal. Removes the upper part of the uterus and leaves the cervix in place.
*Radical. Removes the uterus, the cervix, the upper part of the vagina, and supporting tissues. (This is done in some cases of cancer.)
Often one or both ovaries and fallopian tubes are removed at the same time a hysterectomy is done. For the full article: http://www.4woman.gov/faq/hysterectomy.htm
Hope this helps.
Q. If I Have a Hysterectomy, Will I Go Through Menopause? I am 40 years old and my Doctor said I have to have a Hysterectomy. Does this mean I will go through an early menopause?
After a partial hysterectomy, you’re likely to experience a normal perimenopause and menopause, but it is hard to know when it’s starting because there are no periods to identify the initial changes. Menopause is defined by the cessation of periods for one full year for a woman with a uterus. The cessation of periods is just one point in a process that can take many years. That process still occurs in women who have no uterus, but who still have their ovaries, since it is the ovaries that make most of our sex hormones.
Q. uterine fibroids. Whats the best way to deal with them? My doctor says hysterectomy? What about my hormones?
Surgery is the definitive treatment, especially for complications such as bleeding or pain, and when there's a suspicion for malignancy.
You may read more here: http://www.nlm.nih.gov/medlineplus/ency/article/000914.htm
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp