Medical term:
ThyroShield
potassium
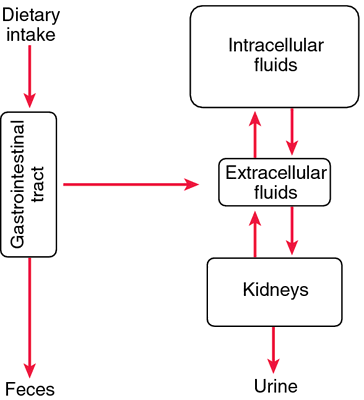
(K) [po-tas´e-um]Since most foods contain a good supply of potassium, potassium deficiency (hypokalemia) is unlikely to be caused by an unbalanced diet. Possible causes include cushing's syndrome (due to an adrenal gland disorder) and fanconi's syndrome (the result of a congenital kidney defect). The cause could also be an excessive dose of cortisone, prolonged vomiting or diarrhea, or thiazide diuretics, which are administered for treatment of hypertension. Signs of potassium deficiency can include weakness and lethargy, rapid pulse, nausea, diarrhea, and tingling sensations.
If the body absorbs enough potassium but the element is not distributed properly, various disorders may develop. Thus an abnormally low content of potassium in the blood may result in an intermittent temporary paralysis of the muscles, known as familial periodic paralysis.
Potassium deficiency can be treated by administration of potassium supplements. There is a large variety of these preparations. Some are liquids, some are powders to be dissolved in liquids, and some are slow-release tablets that dissolve in the intestine. All can cause gastrointestinal irritation. For many persons on diuretic therapy for hypertension, potassium deficiency can be avoided by increasing their consumption of potassium-containing foods, such as bananas, dates, prunes, and raisins, and potassium supplements are not needed. Potassium supplements are never given to patients receiving potassium-sparing diuretics such as amiloride, spironolactone, or triamterene. If the difficulty lies in the body's use of potassium, treatment is concerned with the primary cause of the deficiency.
potassium iodide
Pharmacologic class: Iodine, iodide
Therapeutic class: Antithyroid agent, expectorant
Pregnancy risk category D
Action
Rapidly inhibits thyroid hormone release, reduces thyroid vascularity, and decreases thyroid uptake of radioactive iodine after radiation emergencies or administration of radioactive iodine isotopes. As expectorant, thought to increase respiratory tract secretions, thereby decreasing mucus viscosity.
Availability
Saturated solution (SSKI): 1 g potassium iodide/ml in 30- and 240-ml bottles
Solution (strong iodine solution, Lugol's solution): 5% iodine and 10% potassium iodide in 120-ml bottle
Syrup: 325 mg potassium iodide/5 ml
Tablets: 130 mg (available only through state and federal agencies)
Indications and dosages
➣ Preparation for thyroidectomy
Adults and children: One to five drops SSKI P.O. t.i.d. or three to six drops strong iodine solution P.O. t.i.d. for 10 days before surgery
➣ Thyrotoxic crisis
Adults and children: 500 mg P.O. (approximately 10 drops SSKI) q 4 hours or 1 ml P.O. (strong iodine solution) t.i.d., at least 1 hour after initial propylthiouracil or methimazole dose
➣ Radiation protectant in emergencies
Adults older than age 40 with predicted thyroid exposure of 500 centigrays (cGy), adults ages 18 to 40 with predicted exposure of 10 cGy, pregnant or breastfeeding women with predicted exposure of 5 cGy, and adolescents weighing 70 kg (154 lb) or more with predicted exposure of 5 cGy: 130 mg P.O. (tablet) Children ages 3 to 18 (except adolescents weighing 70 kg [154 lb] or more) with predicted thyroid exposure of 5 cGy: 65 mg P.O. (tablet) Children ages 1 month to 3 years with predicted thyroid exposure of 5 cGy: 32 mg P.O. (tablet)
Infants from birth to age 1 month with predicted thyroid exposure of 5 cGy: 16 mg P.O. (tablet)
➣ Expectorant
Adults: 300 to 650 mg P.O. (SSKI) three or four times daily, given with at least 6 oz of fluid
Children: 60 to 250 mg P.O. (SSKI) q.i.d., given with at least 6 oz of fluid
Off-label uses
• Lymphocutaneous sporotrichosis
Contraindications
• Hypersensitivity to iodine, shellfish, or bisulfites (with some products)
• Hypothyroidism
• Renal impairment
• Acute bronchitis
• Addison's disease
• Acute dehydration
• Heat cramps
• Hyperkalemia
• Tuberculosis
• Iodism
• Concurrent use of potassium-containing drugs, potassium-sparing diuretics, or salt substitutes containing potassium
Precautions
Use cautiously in:
• cystic fibrosis, adolescent acne, hypocomplementemic vasculitis, goiter, autoimmune thyroid disease
• pregnant or breastfeeding patients
• children.
Administration
• Dilute saturated solution with at least 6 oz of water.
☞ Don't give concurrently with other potassium-containing drugs or potassium-sparing diuretics, because of increased risk of hyperkalemia, arrhythmias, and cardiac arrest.
• Know that U.S. government stockpiles potassium iodide 130-mg tablets for emergency use.
• When giving to very young children or patients who can't swallow tablets, crush tablet, dissolve in 20 ml of water, and add 20 ml of selected beverage (such as orange juice).
• Be aware that potassium iodide use as expectorant has been largely replaced by safer and more effective drugs.
Adverse reactions
CNS: confusion; unusual fatigue; paresthesia, pain, or weakness in hands or feet
Metabolic: thyroid hyperplasia, goiter (with prolonged use), thyroid adenoma, severe hypothyroidism, hyperkalemia, iodism (with large doses or prolonged use)
Musculoskeletal: weakness and heaviness of legs
Other: tooth discoloration (with strong iodide solution), hypersensitivity reactions including angioedema, fever, cutaneous and mucosal hemorrhage, serum sickness-like reaction
Interactions
Drug-drug. Lithium, other thyroid drugs: additive hypothyroidism Potassium-sparing diuretics, other potassium preparations: increased risk of hyperkalemia, arrhythmias, and cardiac arrest
Drug-diagnostic tests. Radionuclide thyroid imaging: altered test results Thyroid uptake of131I, 123I, sodium pertechnetate Tc 99m: decreased uptake
Drug-food. Salt substitutes containing potassium: increased risk of hyperkalemia
Patient monitoring
☞ In long-term use, check for signs and symptoms of iodism (metallic taste, sore teeth and gums, sore throat, burning of mouth and throat, coldlike symptoms, severe headache, productive cough, GI irritation, diarrhea, angioedema, rash, fever, and cutaneous or mucosal hemorrhage). Discontinue drug immediately if these occur.
• Monitor potassium level; watch for signs and symptoms of potassium toxicity.
• Assess ECG, renal function, fluid intake and output, and creatinine and blood urea nitrogen levels.
• Monitor thyroid function tests. Watch for evidence of hypothyroidism or hyperthyroidism.
Patient teaching
• Tell patient to dilute in at least 6 oz of water or juice and to take with meals.
• Advise patient to sip strong iodine solution through a straw to help prevent tooth discoloration.
☞ Teach patient to recognize and immediately report signs and symptoms of iodism and potassium toxicity.
• Instruct patient to minimize GI upset by eating small, frequent servings of food and drinking plenty of fluids.
• Inform patient that many salt substitutes are high in potassium. Advise him not to use these without prescriber's approval.
• Caution patient not to take drug if she is pregnant or breastfeeding (except in emergency use).
• As appropriate, review all other significant and life-threatening adverse reactions and interactions, especially those related to the drugs, tests, and foods mentioned above.
potassium iodide
A drug used in the pre-operative management of hyperthyroidism, in the treatment of the fungal infection cutaneous SPOROTRICHOSIS, and to treat iodine deficiency. The drug is on the WHO official list.Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp