Medical term:
antivaricose
Varicose Veins
Definition
Description
Causes and symptoms
Key terms
Diagnosis
Treatment
Prognosis
Resources
Books
varicose
[var´ĭ-kōs]Prolonged periods of standing or sitting without movement place a heavy strain on the veins. Without the massaging action of the muscles, the blood tends to back up. The weight of blood continually pressing downward against closed venous valves causes the veins to distend, and in time they lose their natural elasticity. When a number of valves no longer function efficiently, the blood collects in the veins, which gradually become swollen and more distended. During pregnancy, more force often is necessary to push the blood through the veins because of the pregnant uterus pressing against the veins coming from the legs and preventing the free flow of blood; this increased back pressure can cause varicose veins.
var·i·cose veins
[MIM*192200]varicose veins
Varicosis; varicosity Surgery Enlarged, twisted veins with nonfunctioning valves, resulting in IV pooling of blood and venous enlargement, most commonly in leg veins; VVs affect ±10% of the population, most commonly ♀, age 30 to 60 Etiology Congenital valve defects, thrombophlebitis, pregnancy, prolonged standing or sitting, poor posture, ↑ intraabdominal pressure. See Esophageal varices, Vein stripping. Cf Varicocele.varicose veins
Enlarged, twisted and distorted veins, occurring in the legs, at the lower end of the gullet (see VARICES) or in the scrotum (see VARICOCOELE). Leg varicosities are due to a constitutional or acquired failure of the vein valves so that deep vein pressure is transmitted to the surface veins. They cause stagnation of blood, inadequacy in local tissue nutrition and tissue staining and breakdown to form varicose ulcers. Deep veins, if healthy, afford adequate blood drainage so varicose veins of the legs can safely be removed or obstructed by injections of sclerosing substances. Support from firm elastic hosiery is also helpful. Exercise is beneficial.Varicose Veins
| DRG Category: | 263 |
| Mean LOS: | 6 days |
| Description: | SURGICAL: Vein Ligation and Stripping |
| DRG Category: | 299 |
| Mean LOS: | 5.8 days |
| Description: | MEDICAL: Peripheral Vascular Disorders With Major CC |
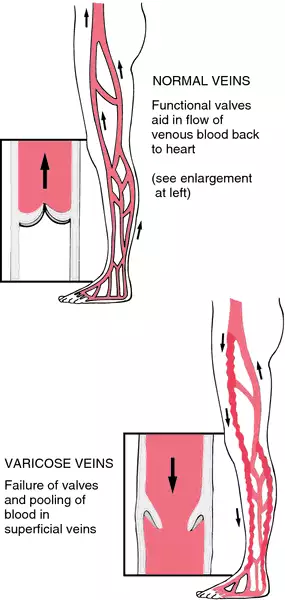
Varicose veins (varicosities) are the visible manifestations of abnormally dilated, tortuous veins. They occur most often in the lower extremities but can appear anywhere in the body. Primary varicosities are caused by incompetent valves in the superficial saphenous veins, whereas secondary varicosities are the result of impaired blood flow in the deep veins. Primary varicosities tend to occur in both legs, whereas secondary varicosities usually occur in only one leg.
In a ladderlike fashion, perforator veins connect the deep vein and the superficial vein systems, promoting drainage of the lower extremities. Blood can be shunted from one system to the other in the event of either system’s being compressed. Incompetence in one system can lead to varicosities. Varicose veins are considered a chronic disease and, along with valvular incompetence, can progress to chronic venous insufficiency (CVI).
Causes
Primary varicose veins occur because of incompetent venous valves that result in venous hypertension. They occur most commonly at the saphenofemoral junction. Several factors cause increased venous pressure and venous stasis that result in dilation and stretching of the vessel wall. Increased venous pressure results from being erect, which shifts the full weight of the venous column of blood to the legs. Prolonged standing increases venous pressure because leg muscle use is less; therefore, blood return to the heart is decreased. Secondary varicose veins result from deep venous thrombosis and its sequelae or congenital anatomical abnormalities.
Heavy lifting, genetic factors, obesity, thrombophlebitis, pregnancy, trauma, abdominal tumors, congenital or acquired arteriovenous fistulae, and congenital venous malformations are among the causes of varicose veins. Chronic liver diseases such as cirrhosis can cause varicosities in the rectum, abdomen, and esophagus.
Genetic considerations
Genetic transmission of varicose veins has been reported since the 1950s with various modes of transmission suggested. Several loci have been identified through linkage analysis (FOXC2, LIPH), and candidate genes are being further investigated. Disruption of production of the gene coding for vascular endothelial growth factor (VEGF) is one implicated mechanism. Family history accounts for an estimated 50% of the risk of disease.
Gender, ethnic/racial, and life span considerations
About 15% to 20% of all adults in the United States have varicose veins. Prevalence increases with age, peaking in the 50s and 60s and decreasing dramatically after age 70. Varicose veins are more common in women; in the population over age 30, four times as many women as men are affected. There are no known ethnic or racial considerations.
Global health considerations
Varicose veins affect an estimated one in five persons in the world. The prevalence of venous disease and varicose veins is higher in developed than in developing nations, likely due to alterations in lifestyle, nutrition, body mass index, and physical activity.
Assessment
History
Elicit a history of symptoms, paying particular attention to pain and discomfort, changes in appearance of vessels and skin, and complaints of a sensation of fullness of the lower extremities. Ask the patient to describe the amount of time each day spent standing. Take an occupational history with particular attention to those jobs that require long hours of walking or standing. Question the patient about lifetime weight changes, such as changes during pregnancy and sustained periods of being overweight. Ask the patient if there is a personal or family history of heart disease, obesity, or varicose veins.
Physical examination
Superficial veins can be inspected for distension and prominence as well as accompanying symptoms such as ulceration, swelling, blanching, and a sense of fullness of the legs. The number, severity, and type of varicosities determine the symptoms experienced by the individual. With the patient standing, examine the legs from the groin to the foot in good lighting. Inspect the ankles, measure the calves for differences, and assess for edema. Time of examination is a factor because secondary varicosities are more symptomatic earlier in the day. Palpate both legs for dilated, bulbous, or corkscrew vessels. Patients may complain of heaviness, aching, edema, muscle cramps, increased fatigue of lower leg muscles, and itching. Severity of discomfort may be difficult to assess and is unrelated to the size of the varicosity.
Psychosocial
The patient with varicose veins has usually been dealing with a progressively worsening condition. Assess the patient for any problems with body image because of the changed appearance of skin surface that is caused by varicose veins. Question the patient to determine possible lifestyle adjustments to decrease symptoms. The patient may need job counseling or occupational retraining.
Diagnostic highlights
General Comments: Incompetency of the deep and superficial veins can be diagnosed by several tests.
| Test | Normal Result | Abnormality With Condition | Explanation |
|---|---|---|---|
| Duplex ultrasound (most commonly used diagnostic tool) | Normal Doppler venous signal with spontaneous respirations; no evidence of occlusion | Reversal of blood flow is noted as a result of incompetent valves in varicose veins | Detects moving red blood cells, thus demonstrating venous patency |
| Trendelenburg’s test | Veins fill from below in about 30 sec after the tourniquet is in place and the client stands; no further blood fills the veins from above after the tourniquet is released | Additional blood flows into the vein from above, indicating a valve is incompetent and has allowed a backflow of blood | Detects abnormal filling time and incompetent valves; veins normally fill from below; if the vein fills from above, the incompetent valve is allowing blood to flow backward |
| Venous plethysmography (cuff pressure test) | Patent venous system without evidence of thrombosis or occlusion | Venous obstruction | Measures the volume of an extremity; rules out a deep vein thrombosis |
| Magnetic resonance venography and magnetic resonance imaging | Normal blood flow without evidence of occlusion | Reversal of blood flow noted | Examines blood flow in extremities |
| Venography | No evidence of obstruction | Abnormal venous flow seen | X-ray study designed to locate thrombi in lower extremities |
Other Tests: Contrast venography and color-flow duplex ultrasonography
Primary nursing diagnosis
Diagnosis
Altered tissue perfusion (peripheral) related to increased venous pressure and obstructionOutcomes
Tissue perfusion: PeripheralInterventions
Circulatory care; Positioning; Pain managementPlanning and implementation
Collaborative
medical.
Treatment for varicose veins is aimed at improving blood flow, reducing injury, and reducing venous pressure. Pharmacologic treatment is not indicated for varicose veins. To give support and promote venous return, physicians recommend wearing elastic stockings. If the varicosities are moderately severe, the physician may recommend antiembolism stockings or elastic bandages or, in severe cases, custom-fitted heavy-weight stockings with graduated pressure. When obesity is a factor, the patient is placed on a weight-loss regimen. Experts also recommend that the patient stop smoking to prevent vasoconstriction of the vessels.A nonsurgical treatment is the use of sclerotherapy for varicose and spider veins. Sclerotherapy is palliative, not curative, and is often done for cosmetic reasons after surgical intervention. A sclerosing agent, such as sodium tetradecyl sulfate (Sotradecol), hypertonic saline, aethoxysclerol, or hyperosmolar salt-sugar solution, is injected into the vein, followed by a compression bandage for a period of time.
surgical.
A surgical approach to varicose veins is vein ligation (tying off) or stripping (removal) of the incompetent veins. Removal of the vein is performed through multiple short incisions from the ankle to the groin. A compression dressing is applied after surgery and is maintained for 3 to 5 days. Patients are encouraged to walk immediately postoperatively. Elevate the foot of the bed 6 to 9 inches to keep the leg above the heart when the postoperative client is in bed.Pharmacologic highlights
No medications are generally used to treat varicose veins, except for analgesics following surgery.
Independent
Nursing interventions are aimed at educating the patient to decrease venous stasis, promote venous return, and prevent tissue injury. To prevent vein distention by compression of superficial veins, teach the patient to apply elastic support stockings before standing and to avoid long periods of standing. The patient should be encouraged to engage in an exercise program of walking to strengthen leg muscles. Teach the patient to avoid crossing the legs when sitting and to elevate the legs when sitting or lying down. The patient should be taught to observe the skin when removing stockings to check for signs of irritation, edema, decreased nerve sensation, and discoloration. Preventive measures are similar to those for a patient with thrombophlebitis.
For patients who have had sclerotherapy, teaching should focus on activity restrictions. The patient should learn to avoid heavy lifting. Teach the patient to wait 24 to 48 hours after the procedure before showering and to avoid tub baths. Teach the patient to wear supportive stockings as ordered. Prepare the patient by advising him or her to expect ecchymosis and some scarring, which will fade in several weeks. Caution the patient that some residual brown staining may remain at the injection sites. Inform the patient that the sclerotherapy may need to be repeated in other areas.
Evidence-Based Practice and Health Policy
Karathanos, C., Sfyroeras, G., Drakou, A., Roussas, N., Exarchou, M., Kyriakou, D., & Giannoukas, A.D. (2012). Superficial vein thrombosis in patients with varicose veins: role of thrombophilia factors, age and body mass. European Journal of Vascular and Endovascular Surgery, 43(3), 355–358.
- In a study among 230 patients with varicose veins, 55.7% experienced a superficial vein thrombosis (SVT).
- Patients older than 60 were 3.56 times more likely to have experienced SVT than patients younger than 60 (95% CI, 1.9 to 6.68; p < 0.001).
- Obese patients were 3.3 times more likely to have experienced SVT than patients of normal weight (95% CI, 1.53 to 7.22; p = 0.002).
Documentation guidelines
- Physical assessment of both extremities: Presence of edema, pain, discoloration
- Reaction to the medications used for sclerotherapy and pain management
- Tolerance to activity and exercise
Discharge and home healthcare guidelines
prevention.
To prevent worsening of varicosities, teach the patient to avoid prolonged standing in one place, to avoid sitting with the legs crossed, to elevate the legs frequently during the day, to wear support stockings as ordered, and to drink 2 to 3 L of fluid daily. The patient should wear shoes that fit comfortably and are not too tight.medications.
Teach the patient the purpose, dosage, route, and side effects of any medications ordered.complications.
Teach the patient to recognize and observe daily for signs of thrombophlebitis, which include redness, local swelling, warmth, discoloration (not related to surgery area), and back pain on bending. Teach the patient which signs to report to the physician.postoperative complications.
Teach the patient to report any signs of infection, such as redness at incision sites or injection sites, severe pain, purulent drainage, fever, or swelling.Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp