Medical term:
electrocardiogram
electrocardiogram
(ECG, EKG) [e-lek″tro-kahr´de-o-gram″]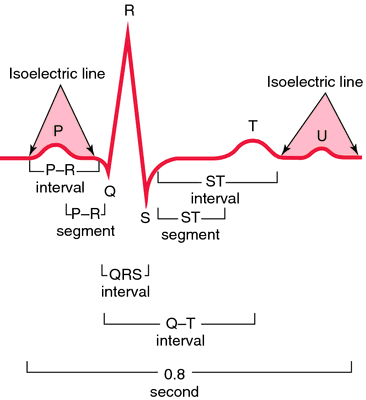
e·lec·tro·car·di·o·gram (ECG, EKG),
(ē-lek'trō-kar'dē-ō-gram), Do not confuse this word with electrocardiograph.electrocardiogram
(ĭ-lĕk′trō-kär′dē-ə-grăm′)electrocardiogram
ECG, EKG Cardiology A non-invasive test of the electrical activity of heart's conduction system, which is transformed into recordings on graph paper–an electrocardiograph; in an EKG, electrodes–leads are placed on 12 specific sites of the body: standard limb leads–I, II, III, augmented limb leads–aVr , aVl, and aVf, and precordial or chest leads–V1 to V6; EKG tracings consist of 3 major components: the P wave, which indicates atrial depolarization, the QRS complex–ventricular depolarization, and the T wave–ventricular repolarization; the Holter monitor is a portable EKG recording device worn by an individual for continuous monitoring; the EKG is used to detect cardiac damage by evaluating alterations in the electrical conduction the heart, and can be performed at rest or during excercise–eg thallium stress test; the Holter monitor is a portable device worn by a Pt for continuous cardiac monitoring; the EKG is used to detect the presence and location of myocardial ischemia or infarction, cardiac hypertrophy, arrhythmias, conduction defects. See His bundle electrocardiography, Signal-averaged electrocardiography, Sleep electrocardiography.e·lec·tro·car·di·o·gram
(ECG, EKG) (ĕ-lek'trō-kahr'dē-ō-gram)electrocardiogram (ECG)
The tracing on paper, representing the electrical events associated with the heartbeats, produced by the ELECTROCARDIOGRAPH.electrocardiogram
see ECG.Electrocardiogram (ECG, EKG)

Electrocardiogram
Common use
Area of application
Heart.Contrast
None.Description
The monitoring of pulse and blood pressure evaluates only the mechanical activity of the heart. The electrocardiogram (ECG), a noninvasive study, measures the electrical currents or impulses that the heart generates during a cardiac cycle (see figure of a normal ECG at end of monograph). Electrical impulses travel through a conduction system beginning with the sinoatrial (SA) node and moving to the atrioventricular (AV) node via internodal pathways. From the AV node, the impulses travel to the bundle of His and onward to the right and left bundle branches. These bundles are located within the right and left ventricles. The impulses continue to the cardiac muscle cells by terminal fibers called Purkinje fibers. The ECG is a graphic display of the electrical activity of the heart, which is analyzed by time intervals and segments. Continuous tracing of the cardiac cycle activity is captured as heart cells are electrically stimulated, causing depolarization and movement of the activity through the cells of the myocardium.
The ECG study is completed by using 12, 15, or 18 electrodes attached to the skin surface to obtain the total electrical activity of the heart. Each lead records the electrical potential between the limbs or between the heart and limbs. The ECG machine records and marks the 12 leads (most common system used) on the strip of paper in the machine in proper sequence, usually 6 in. of the strip for each lead. The ECG pattern, called a heart rhythm, is recorded by a machine as a series of waves, intervals, and segments, each of which pertains to a specific occurrence during the contraction of the heart. The ECG tracings are recorded on graph paper using vertical and horizontal lines for analysis and calculations of time, measured by the vertical lines (1 mm apart and 0.04 sec per line), and of voltage, measured by the horizontal lines (1 mm apart and 0.5 mV per 5 squares). A pulse rate can be calculated from the ECG strip to obtain the beats per minute. The P wave represents the depolarization of the atrial myocardium; the QRS complex represents the depolarization of the ventricular myocardium; the P-R interval represents the time from beginning of the excitation of the atrium to the beginning of the ventricular excitation; and the ST segment has no deflection from baseline, but in an abnormal state may be elevated or depressed. An abnormal rhythm is called an arrhythmia
The ankle-brachial index (ABI) can also be assessed during this study. This noninvasive, simple comparison of blood pressure measurements in the arms and legs can be used to detect peripheral artery disease (PAD). A Doppler stethoscope is used to obtain the systolic pressure in either the dorsalis pedis or the posterior tibial artery. This ankle pressure is then divided by the highest brachial systolic pressure acquired after taking the blood pressure in both arms of the patient. This index should be greater than 1. When the index falls below 0.5, blood flow impairment is considered significant. Patients should be scheduled for a vascular consult for an abnormal ABI. Patients with diabetes or kidney disease, as well as some elderly patients, may have a falsely elevated ABI due to calcifications of the vessels in the ankle causing an increased systolic pressure. The ABI test approaches 95% accuracy in detecting PAD. However, a normal ABI value does not absolutely rule out the possibility of PAD for some individuals, and additional tests should be done to evaluate symptoms.
This procedure is contraindicated for
- N/A
Indications
- Assess the extent of congenital heart disease
- Assess the extent of myocardial infarction (MI) or ischemia, as indicated by abnormal ST segment, interval times, and amplitudes
- Assess the function of heart valves
- Assess global cardiac function
- Detect arrhythmias, as evidenced by abnormal wave deflections
- Detect peripheral artery disease (PAD)
- Detect pericarditis, shown by ST segment changes or shortened P-R interval
- Determine electrolyte imbalances, as evidenced by short or prolonged Q-T interval
- Determine hypertrophy of the chamber of the heart or heart hypertrophy, as evidenced by P or R wave deflections
- Evaluate and monitor cardiac pacemaker function
- Evaluate and monitor the effect of drugs, such as digitalis, antiarrhythmics, or vasodilating agents
- Monitor ECG changes during an exercise test
- Monitor rhythm changes during the recovery phase after an MI
Potential diagnosis
Normal findings
- Normal heart rate according to age: range of 60 to 100 beats/min in adults
- Normal, regular rhythm and wave deflections with normal measurement of ranges of cycle components and height, depth, and duration of complexes as follows:
- P wave: 0.12 sec or three small blocks with amplitude of 2.5 mm
- Q wave: less than 0.04 mm
- R wave: 5 to 27 mm amplitude, depending on lead
- T wave: 1 to 13 mm amplitude, depending on lead
- QRS complex: 0.1 sec or two and a half small blocks
- ST segment: 1 mm
Abnormal findings related to
- Arrhythmias
- Atrial or ventricular hypertrophy
- Bundle branch block
- Electrolyte imbalances
- Heart rate of 40 to 60 beats/min in adults
- MI or ischemia
- PAD
- Pericarditis
- Pulmonary infarction
- P wave: An enlarged P wave deflection could indicate atrial enlargement; an absent or altered P wave could suggest that the electrical impulse did not come from the SA node
- P-R interval: An increased interval could imply a conduction delay in the AV node
- QRS complex: An enlarged Q wave may indicate an old infarction; an enlarged deflection could indicate ventricular hypertrophy; increased time duration may indicate a bundle branch block
- ST segment: A depressed ST segment indicates myocardial ischemia; an elevated ST segment may indicate an acute MI or pericarditis; a prolonged ST segment (or prolonged QT) may indicate hypocalcemia. A shortened ST segment may indicate hypokalemia
- Tachycardia greater than 120 beats/min
- T wave: A flat or inverted T wave may indicate myocardial ischemia, infarction, or hypokalemia; a tall, peaked T wave with a shortened QT interval may indicate hyperkalemia
Critical findings
- Acute changes in ST elevation are usually associated with acute MI or pericarditis.
- Asystole
- Heart block, second- and third-degree with bradycardia less than 60 beats/min
- Pulseless electrical activity
- Pulseless ventricular tachycardia
- Premature ventricular contractions (PVCs) greater than three in a row, pauses greater than 3 sec, or identified blocks
- Unstable tachycardia
- Ventricular fibrillation
- Asystole
- Bradycardia less than 60 beats/min
- Pulseless electrical activity
- Pulseless ventricular tachycardia
- Supraventricular tachycardia
- Ventricular fibrillation
It is essential that a critical finding be communicated immediately to the requesting health-care provider (HCP). A listing of these findings varies among facilities.
Timely notification of a critical finding for lab or diagnostic studies is a role expectation of the professional nurse. Notification processes will vary among facilities. Upon receipt of the critical value the information should be read back to the caller to verify accuracy. Most policies require immediate notification of the primary HCP, Hospitalist, or on-call HCP. Reported information includes the patient’s name, unique identifiers, critical value, name of the person giving the report, and name of the person receiving the report. Documentation of notification should be made in the medical record with the name of the HCP notified, time and date of notification, and any orders received. Any delay in a timely report of a critical finding may require completion of a notification form with review by Risk Management.
Adult
Pediatric
Interfering factors
Factors that may impair the results of the examination
- Anatomic variation of the heart (i.e., the heart may be rotated in both the horizontal and frontal planes).
- Distortion of cardiac cycles due to age, gender, weight, or a medical condition (e.g., infants, women [may exhibit slight ST segment depression], obese patients, pregnant patients, patients with ascites).
- High intake of carbohydrates or electrolyte imbalances of potassium or calcium.
- Improper placement of electrodes or inadequate contact between skin and electrodes because of insufficient conductive gel or poor placement, which can cause ECG tracing problems.
- ECG machine malfunction or interference from electromagnetic waves in the vicinity.
- Inability of the patient to remain still during the procedure, because movement, muscle tremor, or twitching can affect accurate test recording.
- Increased patient anxiety, causing hyperventilation or deep respirations.
- Medications such as barbiturates and digitalis.
- Strenuous exercise before the procedure.
Nursing Implications and Procedure
Pretest
- Positively identify the patient using at least two unique identifiers before providing care, treatment, or services.
- Patient Teaching: Inform the patient this procedure can assist in assessing cardiac (heart) function.
- Obtain a history of the patient’s complaints or clinical symptoms, including a list of known allergens, especially allergies or sensitivities to latex, anesthetics, or sedatives. Ask if the patient has had a heart transplant, implanted pacemaker, or internal cardiac defibrillator.
- Obtain a history of the patient’s cardiovascular system, symptoms, and results of previously performed laboratory tests and diagnostic and surgical procedures.
- Obtain a list of the patient’s current medications, including herbs, nutritional supplements, and nutraceuticals (see Effects of Natural Products on Laboratory Values online at DavisPlus).
- Review the procedure with the patient. Inform the patient that it may be necessary to remove hair from the site before the procedure. Address concerns about pain related to the procedure and explain that there should be no discomfort related to the procedure. Inform the patient that the procedure is performed by an HCP and takes approximately 15 min.
- Sensitivity to social and cultural issues, as well as concern for modesty, is important in providing psychological support before, during, and after the procedure.
- Instruct the patient to remove jewelry and other metallic objects from the area to be examined.
- Note that there are no food, fluid, or medication restrictions unless by medical direction.
Intratest
- Potential complications: N/A
- Observe standard precautions, and follow the general guidelines in Patient Preparation and Specimen Collection. Positively identify the patient.
- Ensure the patient has complied with pretesting preparations.
- Ensure the patient has removed all external metallic objects from the area to be examined prior to the procedure.
- Instruct the patient to void prior to the procedure and to change into the gown, robe, and foot coverings provided.
- Record baseline values.
- Place patient in a supine position. Expose and appropriately drape the chest, arms, and legs.
- Instruct the patient to cooperate fully and to follow directions. Instruct the patient to remain still throughout the procedure because movement produces unreliable results.
- Prepare the skin surface with alcohol and remove excess hair. Use clippers to remove hair from the site, if appropriate. Dry skin sites.
- Avoid the use of equipment containing latex if the patient has a history of allergic reaction to latex.
- Apply the electrodes in the proper position. When placing the six unipolar chest leads, place V1 at the fourth intercostal space at the border of the right sternum, V2 at the fourth intercostal space at the border of the left sternum, V3 between V2 and V4, V4 at the fifth intercostal space at the midclavicular line, V5 at the left anterior axillary line at the level of V4 horizontally, and V6 at the level of V4 horizontally and at the left midaxillary line. The wires are connected to the matched electrodes and the ECG machine. Chest leads (V1, V2, V3, V4, V5, and V6) record data from the horizontal plane of the heart.
- Place three limb bipolar leads (two electrodes combined for each) on the arms and legs. Lead I is the combination of two arm electrodes, lead II is the combination of right arm and left leg electrodes, and lead III is the combination of left arm and left leg electrodes. Limb leads (I, II, III, aVl, aVf, and aVr) record data from the frontal plane of the heart.
- The machine is set and turned on after the electrodes, grounding, connections, paper supply, computer, and data storage device are checked.
- If the patient has any chest discomfort or pain during the procedure, mark the ECG strip indicating that occurrence.
Post-Test
- Inform the patient that a report of the results will be made available to the requesting HCP, who will discuss the results with the patient.
- When the procedure is complete, remove the electrodes and clean the skin where the electrode was applied.
- Evaluate the results in relation to previously performed ECGs. Denote cardiac rhythm abnormalities on the strip.
- Monitor vital signs and compare with baseline values. Protocols may vary among facilities.
- Instruct the patient to immediately notify an HCP of chest pain, changes in pulse rate, or shortness of breath.
- Recognize anxiety related to the test results and be supportive of perceived loss of independence and fear of shortened life expectancy. Discuss the implications of abnormal test results on the patient’s lifestyle. Provide teaching and information regarding the clinical implications of the test results, as appropriate.
- Nutritional Considerations: Abnormal findings may be associated with cardiovascular disease. Nutritional therapy is recommended for the patient identified to be at risk for developing coronary artery disease (CAD) or for individuals who have specific risk factors and/or existing medical conditions (e.g., elevated LDL cholesterol levels, other lipid disorders, insulin-dependent diabetes, insulin resistance, or metabolic syndrome). Other changeable risk factors warranting patient education include strategies to encourage patients, especially those who are overweight and with high blood pressure, to safely decrease sodium intake, achieve a normal weight, ensure regular participation of moderate aerobic physical activity three to four times per week, eliminate tobacco use, and adhere to a heart-healthy diet. If triglycerides also are elevated, the patient should be advised to eliminate or reduce alcohol. The 2013 Guideline on Lifestyle Management to Reduce Cardiovascular Risk published by the American College of Cardiology (ACC) and the American Heart Association (AHA) in conjunction with the National Heart, Lung, and Blood Institute (NHLBI) recommends a “Mediterranean”-style diet rather than a low-fat diet. The new guideline emphasizes inclusion of vegetables, whole grains, fruits, low-fat dairy, nuts, legumes, and nontropical vegetable oils (e.g., olive, canola, peanut, sunflower, flaxseed) along with fish and lean poultry. A similar dietary pattern known as the Dietary Approach to Stop Hypertension (DASH) makes additional recommendations for the reduction of dietary sodium. Both dietary styles emphasize a reduction in consumption of red meats, which are high in saturated fats and cholesterol, and other foods containing sugar, saturated fats, trans fats, and sodium.
- Social and Cultural Considerations: Numerous studies point to the prevalence of excess body weight in American children and adolescents. Experts estimate that obesity is present in 25% of the population ages 6 to 11 yr. The medical, social, and emotional consequences of excess body weight are significant. Special attention should be given to instructing the child and caregiver regarding health risks and weight control education.
- Recognize anxiety related to test results, and be supportive of fear of shortened life expectancy. Discuss the implications of abnormal test results on the patient’s lifestyle. Provide teaching and information regarding the clinical implications of the test results, as appropriate. Educate the patient regarding access to counseling services. Provide contact information, if desired, for the American Heart Association (www.americanheart.org), the NHLBI (www.nhlbi.nih.gov), or the Legs for Life (www.legsforlife.org).
- Reinforce information given by the patient’s HCP regarding further testing, treatment, or referral to another HCP. Answer any questions or address any concerns voiced by the patient or family.
- Depending on the results of this procedure, additional testing may be performed to evaluate or monitor progression of the disease process and determine the need for a change in therapy. Evaluate test results in relation to the patient’s symptoms and other tests performed.
Related Monographs
- Related tests include antiarrhythmic drugs, apolipoprotein A and B, AST, atrial natriuretic peptide, BNP, blood gases, blood pool imaging, calcium, chest x-ray, cholesterol (total, HDL, LDL), CT cardiac scoring, CT thorax, CRP, CK and isoenzymes, echocardiography, echocardiography transesophageal, exercise stress test, glucose, glycated hemoglobin, Holter monitor, homocysteine, ketones, LDH and isos, lipoprotein electrophoresis, lung perfusion scan, magnesium, MRI chest, MI infarct scan, myocardial perfusion heart scan, myoglobin, PET heart, potassium, pulse oximetry, sodium, triglycerides, and troponin.
- Refer to the Cardiovascular System table at the end of the book for related tests by body system.
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp