Medical term:
mastectomy
Mastectomy
Definition
Mastectomy is the surgical removal of the breast for the treatment or prevention of breast cancer.
Purpose
Mastectomy is performed as a surgical treatment for breast cancer. The severity of a breast cancer is evaluated according to a complex system called staging. This takes into account the size of the tumor and whether it has spread to the lymph nodes, adjacent tissues, and/or distant parts of the body. A mastectomy usually is the recommended surgery for more advanced breast cancers. Women with earlier stage breast cancers, who might also have breast-conserving surgery (lumpectomy), may choose to have a mastectomy. In the United States, approximately 50,000 women a year undergo mastectomy.
The size, location, and type of tumor are important considerations when choosing the best surgery to treat breast cancer. The size of the breast also is an important factor. A woman's psychological concerns and lifestyle choices also should be considered when making a decision.
There are many factors that may make a mastectomy the treatment of choice for a patient. Large tumors are difficult to remove with good cosmetic results. This is especially true if the woman has small breasts. Sometimes multiple areas of cancer are found in one breast, making removal of the whole breast necessary. The surgeon sometimes is unable to remove the tumor with a sufficient amount, or margin, of normal tissue surrounding it. In this situation, the entire breast needs to be removed. Recurrence of breast cancer after a lumpectomy is another indication for mastectomy.
Radiation therapy is almost always recommended following a lumpectomy. If a woman is unable to have radiation, a mastectomy is the treatment of choice. Pregnant women cannot have radiation therapy for fear of harming the fetus. A woman with certain collagen vascular diseases, such as systemic lupus erythematosus or scleroderma, would experience unacceptable scarring and damage to her connective tissue from radiation exposure. Any woman who has had therapeutic radiation to the chest area for other reasons cannot tolerate additional exposure for breast cancer therapy.
The need for radiation therapy after breast conserving surgery may make mastectomy more appealing for nonmedical reasons. Some women fear radiation and choose the more extensive surgery so radiation treatment will not be required. The commitment of time, usually five days a week for six weeks, may not be acceptable for other women. This may be due to financial, personal, or job-related factors. In geographically isolated areas, a course of radiation therapy may require lengthy travel and perhaps unacceptable amounts of time away from family or other responsibilities.
Some women choose mastectomy because they strongly fear recurrence of the breast cancer, and lumpectomy seems too risky. Keeping a breast that has contained cancer may feel uncomfortable for some patients. They prefer mastectomy, so the entire breast will be removed. However, studies have shown that survival rates for women choosing mastectomy and those under-going breast-conserving surgery have been the same.
The issue of prophylactic or preventive mastectomy, or removal of the breast to prevent future breast cancer, is controversial. Women with a strong family history of breast cancer and/or who test positive for a known cancer-causing gene may choose to have both breasts removed. Patients who have had certain types of breast cancers that are more likely to recur may elect to have the unaffected breast removed. Although there is some evidence that this procedure can decrease the chances of developing breast cancer, it is not a guarantee. It is not possible to guarantee that all breast tissue has been removed. There have been cases of breast cancers occurring after both breasts have been removed.
Studies have shown that women who choose preventive mastectomy generally are satisfied with their choice, but also believe they lacked enough information before deciding, particularly about the surgery, genetic testing, and breast reconstruction. A study  released in 2003 concerning women who underwent radical mastectomy of one breast and chose surgical removal of the other breast as a preventive measure found that 83% were highly satisfied with their decision.
released in 2003 concerning women who underwent radical mastectomy of one breast and chose surgical removal of the other breast as a preventive measure found that 83% were highly satisfied with their decision.
There are four types of mastectomies: partial mastectomy, or lumpectomy, in which the tumor and surrounding tissue is removed; simple mastectomy, where the entire breast and some axillary lymph nodes are removed; modified radical mastectomy, in which the entire breast and all axillary lymph nodes are removed; and the radical mastectomy, where the entire breast, axillary lymph nodes, and chest muscles are removed.
(Illustration by Electronic Illustrators Group.)
Precautions
The decision to have mastectomy or lumpectomy should be carefully considered. It is important that the woman be fully informed of all the potential risks and benefits of each surgical treatment before making a choice.
Description
There are several types of mastectomies. The radical mastectomy, also called the Halsted mastectomy, is rarely performed today. It was developed in the late 1800s, when it was thought that more extensive surgery was most likely to cure cancer. A radical mastectomy involves removal of the breast, all surrounding lymph nodes up to the collarbone, and the underlying chest muscle. Women often were left disfigured and disabled, with a large defect in the chest wall requiring skin grafting, and significantly decreased arm sensation and motion. Unfortunately, and inaccurately, it still is the operation many women picture when the word mastectomy is mentioned.
Surgery that removes breast tissue, nipple, an ellipse of skin, and some axillary or underarm lymph nodes, but leaves the chest muscle intact, usually is called a modified radical mastectomy. This is the most common type of mastectomy performed today. The surgery leaves a woman with a more normal chest shape than the older radical mastectomy procedure, and a scar that is not visible in most clothing. It also allows for immediate or delayed breast reconstruction.
In a simple mastectomy, only the breast tissue, nipple, and a small piece of overlying skin are removed. If a few of the axillary lymph nodes closest to the breast also are taken out, the surgery may be called an extended simple mastectomy.
There are other variations on the term mastectomy. A skin-sparing mastectomy uses special techniques that preserve the patient's breast skin for use in reconstruction, although the nipple still is removed. Total mastectomy is a confusing expression, as it may be used to refer to a modified radical mastectomy or a simple mastectomy. In 2003, surgeons reported on a new technique that spared the nipple in many women with early stage breast cancer.
Many women choose to have breast reconstruction performed in conjunction with the mastectomy. The reconstruction can be done using a woman's own abdominal tissue, or using saline-filled artificial expanders, which leave the breast relatively flat but partially reconstructed. Additionally, there are psychological benefits to coming out of the surgery with the first step to a reconstructed breast. Immediate reconstruction will add time and cost to the mastectomy procedure, but the patient can avoid the physical impact of a later surgery.
A mastectomy typically is performed in a hospital setting, but specialized outpatient facilities sometimes are used. The surgery is done under general anesthesia. The type and location of the incision may vary according to plans for reconstruction or other factors, such as old scars. As much breast tissue as possible is removed. Approximately 10 to 20 axillary lymph nodes usually are removed. All tissue is sent to the pathology laboratory for analysis. If no immediate reconstruction is planned, surgical drains are left in place to prevent fluid accumulation. The skin is sutured and bandages are applied.
The surgery may take from two to five hours. Patients usually stay at least one night in the hospital, although outpatient mastectomy is increasingly performed for about 10% of all patients. Insurance usually covers the cost of mastectomy. If immediate reconstruction is performed, the length of stay, recovery period, insurance reimbursement, and fees will vary. In 1998, the Women's Health and Cancer Rights Act required insurance plans to cover the cost of breast reconstruction in conjunction with a mastectomy procedure.
Preparation
Routine preoperative preparations, such as not eating or drinking the night before surgery, typically are ordered for a mastectomy. On rare occasions, the patient also may be asked to donate blood in case a blood transfusion is required during surgery. The patient should advise the surgeon of any medications she is taking. Information regarding expected outcomes and potential complications also should be part of preparation for a mastectomy, as for any surgical procedure. It is especially important that women know about sensations they might experience after surgery, so they are not misinterpreted as a sign of poor wound healing or recurrent cancer.
Aftercare
In the past, women often stayed in the hospital at least several days. Now many patients go home the same day or within a day or two after their mastectomies. Visits from home care nurses can sometimes be arranged, but patients need to learn how to care for themselves before discharge from the hospital. Patients may need to learn to change bandages and/or care for the incision. The surgical drains must be attended to properly; this includes emptying the drain, measuring fluid output, moving clots through the drain, and identifying problems that need attention from the doctor or nurse. If the drain becomes blocked, fluid or blood may collect at the surgical site. Left untreated, this accumulation may cause infection and/or delayed wound healing.
After a mastectomy, activities such as driving may be restricted according to individual needs. Pain is usually well controlled with prescribed medication. Severe pain may be a sign of complications, and should be reported to the physician. A return visit to the surgeon is usually scheduled 7 to 10 days after the procedure.
Exercises to maintain shoulder and arm mobility may be prescribed as early as 24 hours after surgery. These are very important in restoring strength and promoting good circulation. However, intense exercise should be avoided for a time after surgery in order to prevent injury. The specific exercises suggested by the physician will change as healing progresses. Physical therapy is an integral part of care after a mastectomy, aiding in the overall recovery process.
Emotional care is another important aspect of recovery from a mastectomy. A mastectomy patient may feel a range of emotions including depression, negative self-image, grief, fear and anxiety about possible recurrence of the cancer, anger, or guilt. Patients are advised to seek counseling and/or support groups and to express their emotions to others, whether family, friends, or therapists. Assistance in dealing with the psychological effects of the breast cancer diagnosis, as well as the surgery, can be invaluable for women.
Measures to prevent injury or infection to the affected arm should be taken, especially if axillary lymph nodes were removed. There are a number of specific instructions directed toward avoiding pressure or constriction of the arm. Extra care must be exercised to avoid injury, to treat it properly if it occurs, and to seek medical attention promptly when appropriate.
Additional treatment for breast cancer may be necessary after a mastectomy. Depending on the type of tumor, lymph node status, and other factors, chemotherapy, radiation therapy, and/or hormone therapy may be prescribed.
Risks
Risks that are common to any surgical procedure include bleeding, infection, anesthesia reaction, or unexpected scarring. After mastectomy and axillary lymph node dissection, a number of complications are possible. A woman may experience decreased feeling in the back of her armpit or other sensations including numbness, tingling, or increased skin sensitivity. Some women report phantom breast symptoms, experiencing itching, aching, or other sensations in the breast that has been removed. There may be scarring around where the lymph nodes were removed, resulting in decreased arm mobility and requiring more intense physical therapy.
Approximately 10% to 20% of patients develop lymphedema after axillary lymph node removal. This swelling of the arm, caused by faulty lymph drainage, can range from mild to severe. It can be treated with elevation, elastic bandages, and specialized physical therapy. Lymphedema is a chronic condition that requires continuing treatment. This complication can arise at any time, even years after surgery. A new technique called sentinel lymph node mapping and biopsy often eliminates the need for removing some or all lymph nodes by testing the first lymph node for cancer.
Normal results
A mastectomy is performed as the definitive surgical treatment for breast cancer. The goal of the procedure is that the breast cancer is completely removed and does not recur.
Abnormal results
An abnormal result of a mastectomy is the incomplete removal of the breast cancer or a recurrence of the cancer. Other abnormal results include long-lasting (chronic) pain or impairment that does not improve after several months of physical therapy.
Resources
Periodicals
"American Women Still Having Too Many Mastectomies." Women's Health Weekly February 6, 2003: 10.
Frost, Marlene, et al. "Long-term Satisfaction and Psychological and Social Function Following Bilateral Prophylactic Mastectomy." Journal of the American Medical Association July 20, 2000: 319-24.
"Majority Satisfied with Prophylactic Mastectomy Decision." AORN Journal November 2003: 773.
"Studies Compare Mastectomy, Lumpectomy Survival Rates." Clinican Reviews January 2003: 24.
Organizations
American Cancer Society. 1599 Clifton Rd., NE, Atlanta, GA 30329-4251. (800) 227-2345. http://www.cancer.org.
National Lymphedema Network. 2211 Post St., Suite 404, San Francisco, CA 94115-3427. (800) 541-3259 or (415) 921-1306. 〈http://www.wenet.net/∼lymphnet/〉.
Y-ME National Organization for Breast Cancer Information and Support. 18220 Harwood Ave., Homewood, IL 60430. 24-hour hotlines: (800) 221-2141 or (708) 799-8228.
Other
ibreast.org April 15, 2001. [cited June 12, 2001]. http://www.breastcancer.org.
Living Beyond Breast Cancer April 15, 2001. [cited June 12, 2001]. http://www.lbbc.org.
Key terms
Axillary — Located in or near the armpit.
Lymphedema — Swelling caused by an accumulation of fluid from faulty lymph drainage.
Mastectomy, modified radical — Total mastectomy with axillary lymph node dissection, but with preservation of the pectoral muscles.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
mastectomy
[mas-tek´to-me]surgical removal of breast tissue, usually for treatment of malignant breast tumors, although occasionally this may be advisable for benign tumors, other diseases of the breast such as fibrocystic disease of the breast, or prophylaxis. Patients with breast disorders should be informed about all the options for treatment including alternatives to mastectomy. Types of mastectomy include the simple or total mastectomy and radical, modified radical, and extended radical mastectomies.
Patient Care. The psychological aspects of the breast must always be considered in the care of women who face the prospect of loss of breast tissue through surgery. The breast is symbolic of femininity, motherhood, and sexual attractiveness for some individuals. Psychological problems likely to be associated with mastectomy include disturbance in self-concept related to changes in body image, self-esteem, role performance, and personal identity. Newer, less mutilating surgical procedures and cosmetically successful reconstructive plastic surgery (mammaplasty) to replace surgically removed breast tissue have diminished some of the emotional trauma formerly associated with mastectomy.
Following mastectomy the patient is likely to experience such physical problems as pain, numbness, tingling, and weakness related to nerve damage and muscle atrophy. Additionally, the patient is subject to lymphedema and collections of serous fluid (seroma) associated with interruption of the flow of lymph.
In addition to routine postoperative care to prevent pulmonary and circulatory complications, the patient must be watched for the development of localized edema, especially if lymph nodes have been removed. In order to provide adequate drainage of serosanguineous fluid that could delay healing of the operative site, the surgeon may insert a flat, narrow drain with multiple openings. The device is part of a portable self-contained closed-suction system that exerts negative pressure. Systems of this kind include Hemovac and Reliavac.
The patient receives routine postoperative care, including coughing and deep-breathing exercises, to prevent respiratory complications and early ambulation to avoid circulatory stasis. When helping the patient from bed it is important to realize that her sense of balance may be impaired because of changes in upper body structures and some hesitancy to use the arm on the operative side to support herself and maintain balance.
Postoperative care should include periodic assessment of sensations (e.g., “phantom breast” sensations) and of functional limitations in the chest wall and affected arm. Additionally numbness, patterns of weakness, and paresthesias are evaluated. The patient should be taught how to recognize and report these symptoms and any changes noted, as they could indicate progressive nerve damage.
Impairment of lymph flow increases the risk of infection. Loss of sensation could predispose the patient to injury from burns, cuts, and other accidental trauma. Venipunctures are not done and blood pressure cuffs are not applied on the arm on the affected side. Prior to discharge the patient is given instruction in ways to avoid trauma: for example, do not carry a heavy handbag or other heavy articles with the affected arm, avoid excessive exposure to sun, do not pick or cut cuticles, and consult the physician or nurse before having vaccinations or injections in the affected arm. Exercises to improve mobility and lymphatic drainage are begun while the patient is in the hospital and continued by her after discharge. These exercises are described and illustrated in the booklet “Help Yourself to Recovery,” which is available from local offices of the American Cancer Society. The Cancer Society also has self-help support groups, called Reach for Recovery, for women following mastectomy.
The woman is encouraged to continue follow-up care, including a clinical breast exam every 3 to 4 months for the first 3 years, then every 6 months for 2 years, and thereafter every 6 to 12 months. Annual mammograms should be obtained and the woman should perform breast self-exams monthly.
Following mastectomy the patient is likely to experience such physical problems as pain, numbness, tingling, and weakness related to nerve damage and muscle atrophy. Additionally, the patient is subject to lymphedema and collections of serous fluid (seroma) associated with interruption of the flow of lymph.
In addition to routine postoperative care to prevent pulmonary and circulatory complications, the patient must be watched for the development of localized edema, especially if lymph nodes have been removed. In order to provide adequate drainage of serosanguineous fluid that could delay healing of the operative site, the surgeon may insert a flat, narrow drain with multiple openings. The device is part of a portable self-contained closed-suction system that exerts negative pressure. Systems of this kind include Hemovac and Reliavac.
The patient receives routine postoperative care, including coughing and deep-breathing exercises, to prevent respiratory complications and early ambulation to avoid circulatory stasis. When helping the patient from bed it is important to realize that her sense of balance may be impaired because of changes in upper body structures and some hesitancy to use the arm on the operative side to support herself and maintain balance.
Postoperative care should include periodic assessment of sensations (e.g., “phantom breast” sensations) and of functional limitations in the chest wall and affected arm. Additionally numbness, patterns of weakness, and paresthesias are evaluated. The patient should be taught how to recognize and report these symptoms and any changes noted, as they could indicate progressive nerve damage.
Impairment of lymph flow increases the risk of infection. Loss of sensation could predispose the patient to injury from burns, cuts, and other accidental trauma. Venipunctures are not done and blood pressure cuffs are not applied on the arm on the affected side. Prior to discharge the patient is given instruction in ways to avoid trauma: for example, do not carry a heavy handbag or other heavy articles with the affected arm, avoid excessive exposure to sun, do not pick or cut cuticles, and consult the physician or nurse before having vaccinations or injections in the affected arm. Exercises to improve mobility and lymphatic drainage are begun while the patient is in the hospital and continued by her after discharge. These exercises are described and illustrated in the booklet “Help Yourself to Recovery,” which is available from local offices of the American Cancer Society. The Cancer Society also has self-help support groups, called Reach for Recovery, for women following mastectomy.
The woman is encouraged to continue follow-up care, including a clinical breast exam every 3 to 4 months for the first 3 years, then every 6 months for 2 years, and thereafter every 6 to 12 months. Annual mammograms should be obtained and the woman should perform breast self-exams monthly.
Halsted mastectomy radical mastectomy.
partial mastectomy removal of the tumor, along with varying amounts of surrounding normal tissue. See also lumpectomy and quadrantectomy. Called also segmental mastectomy.
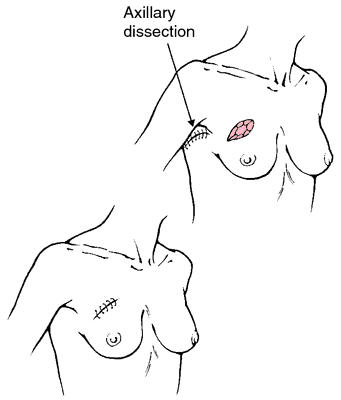
radical mastectomy removal of the breast, pectoral muscles, axillary lymph nodes, and associated skin and subcutaneous tissue in treatment of breast cancer.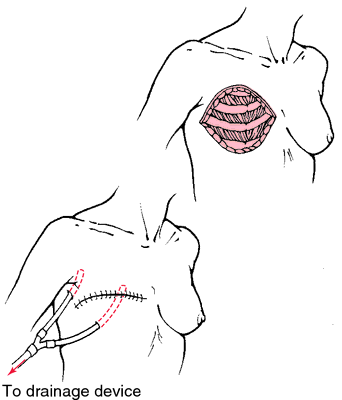
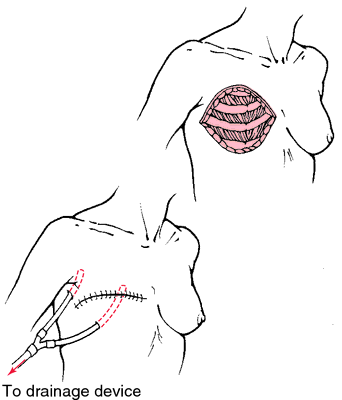
In a radical mastectomy, breast tissue, nipple, underlying muscles, and lymph nodes are removed. From Ignatavicius and Workman, 2001.
radical mastectomy, extended supraradical mastectomy; surgical removal of the internal mammary chain of lymph nodes, the entire involved breast, the underlying chest muscles, and the lymph nodes in the axilla.
radical mastectomy, modified surgical removal of the entire involved breast, and many lymph nodes in the axilla. The underlying chest muscles are removed in part or are left in place after removal of axillary lymph nodes.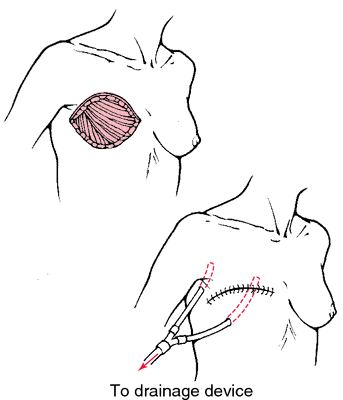
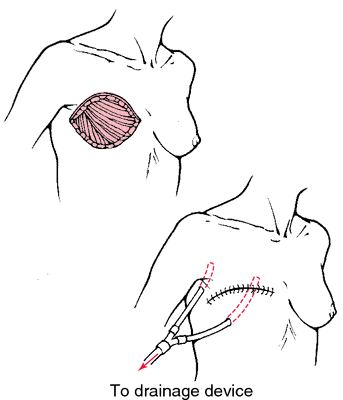
In a modified radical mastectomy, breast tissue, nipple, and lymph nodes are removed, but muscles are left intact. From Ignatavicius and Workman, 2001.
segmental mastectomy partial mastectomy.
simple mastectomy surgical removal of the entire involved breast; the underlying chest muscles and axillary lymph nodes are not removed. More recently called total mastectomy.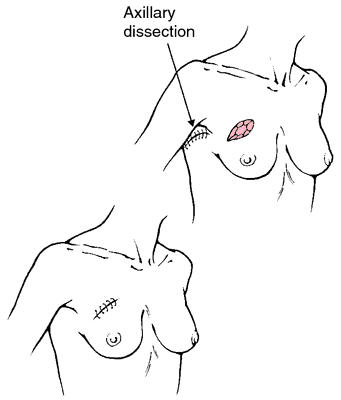
In a simple mastectomy, breast tissue and (usually) nipple are removed, but lymph nodes are left intact. From Ignatavicius and Workman, 2001.
subcutaneous mastectomy excision of breast tissue with preservation of overlying skin, nipple, and areola so that the breast form may be reconstructed.
supraradical mastectomy extended radical mastectomy.
total mastectomy simple mastectomy.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
mas·tec·to·my
(mas-tek'tŏ-mē),Excision of the breast.
Synonym(s): mammectomy
[masto- + G. ektomē, excision]
Farlex Partner Medical Dictionary © Farlex 2012
mastectomy
(mă-stĕk′tə-mē)n. pl. mastecto·mies
Surgical removal of all or part of a breast, sometimes including excision of the underlying pectoral muscles, associated skin, and regional lymph nodes, usually performed as a treatment for cancer.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
mastectomy
The removal of the breast, or as much breast tissue as possible, usually understood to be as part of treatment for breast cancer.Mastectomy for breast cancer is recommended in patients who:
▪ are < age 50;
▪ have a high (histologic) grade cancer;
▪ have a large (> 30 mm) tumour.
Segen's Medical Dictionary. © 2012 Farlex, Inc. All rights reserved.
mastectomy
Surgery The removal of the breast or as much of breast tissue as possible. See Bilateral mastectomy, Extended radical mastectomy, Modified radical mastectomy, Outpatient mastectomy, Partial mastectomy, Prophylactic mastectomy, Radical mastectomy, Simple mastectomy, Subcutaneous mastectomy.McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
mas·tec·to·my
(mas-tek'tŏ-mē)Excision of the breast.
Synonym(s): mammectomy.
Synonym(s): mammectomy.
[masto- + G. ektomē, excision]
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
mastectomy
Surgical removal of the breast (mammary gland). This is done almost exclusively for the treatment of cancer. Radical mastectomy, now a relatively uncommon operation, involves the removal of all breast tissue and skin, the underlying pectoral muscles and the lymph nodes in the armpit. In simple mastectomy, only the breast tissue is removed. In lumpectomy only the obvious mass is removed through a short radial incision.Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005
Patient discussion about mastectomy
Q. Is there any chances of breast cancer recurrence after mastectomy and to what extent? hi guys…..please clarify ……Is there any chances of breast cancer recurrence after mastectomy and to what extent?
A. Yes, there are chances of breast cancer recurrence. Every one out of 13 patient had a chance for it to recur within 10 years mostly at the same place. It can also spread to other parts even. Recurrence among the patients with breast removal is also found but its chances are very less and its risk reduces to below 80%.
More discussions about mastectomyThis content is provided by iMedix and is subject to iMedix Terms. The Questions and Answers are not endorsed or recommended and are made available by patients, not doctors.
Latest Searches:
zoopharmacy - zoopharmacology - zoophagous - zoopery - zooperal - zoopathology - zooparasitica - zooparasitic - zooparasite - zoonotic - zoonosology - Zoonosis - zoonoses - zoonomy - zoonite - zoonerythrin - zoomastigophorean - Zoomastigophorea - Zoomastigophora - zoomania -
- Service manuals - MBI Corp