Medical term:
osteoporotic
os·te·o·po·rot·ic
(os'tē-ō-pŏ-rot'ik),os·te·o·po·rot·ic
(os'tē-ō-pŏr-ot'ik)osteoporosis
(os?te-o-po-ro'sis) [ osteo- + -porosis]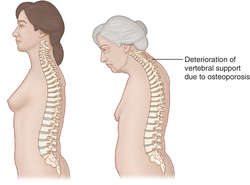
Etiology
Several modifiable factors contribute to bone mass and strength: increased body weight, higher levels of sex hormones, and frequent weight-bearing exercise all build up bone and prevent fractures. Bone loss and the risk of fractures increase with age, immobilization, excess of thyroid hormone, use of corticosteroids and some anticonvulsant drugs, the consumption of alcohol, tobacco, and caffeine, and after menopause. Genetics (a nonmodifiable risk factor) also contributes to osteoporosis. See: table
Symptoms
Bone loss progresses for many years without causing symptoms. When it results in fractures, bone pain and loss of mobility may be disabling. Signs of osteoporosis include deformities of the skeleton, e.g., kyphosis (“dowager’s hump”), and loss of height, esp. if vertebral compression fractures occur.
Treatment
Supplemental calcium and regular exercise help slow or prevent the rate of bone loss and are recommended for most men and women. Bisphosphonate drugs, e.g., alendronate, calcitonin, sodium fluoride, and other agents are useful for patients of both sexes. In menopausal women, estrogen supplementation or the selective estrogen receptor modulators help prevent bone loss and fractures, but calcium supplementation has not been shown to be helpful.
Patient care
Protection against osteoporosis should begin in childhood and adolescence and focus on building bone mass. Children should be encouraged to eat foods rich in calcium; parents should be taught to encourage regular exercise, including school gym classes and sports programs, to build strong bones and establish healthy habits. Parents should also be informed about the effects that eating disorders, excessive dieting, excessive exercise, alcohol consumption, and smoking have on bone density. From the mid-20s through age 35, focus continues to be placed on building and maintaining bone mass through a calcium-rich diet. After age 35, bone resorption exceeds bone formation. Emphasis is placed on preventing bone loss through a healthy diet, use of calcium (plus vitamin D) supplements (an intake of at least 1000 mg of calcium per day), and weight-bearing exercises, e.g., weight-lifting, walking, jogging, dancing, and climbing stairs. High-impact aerobics may create too much stress on the bones of older adults and should be avoided.
After patients have been diagnosed with osteoporosis, time should be spent assessing their diets and activity levels. Although patients should engage in walking or other weight-bearing activity for 30 to 60 min three to four times a week, this goal may need to be approached slowly. Foods rich in calcium include dairy products, spinach, sardines, and nuts. Calcium supplements totaling 1000 to 1500 mg per day should be consumed and can prevent further bone loss. Based on bone density testing, alendronate or another drug that inhibits bone resorption may be prescribed in a daily or weekly formulation. Bisphosphonates like alendronate should be taken on an empty stomach with a full glass (8 oz) of water. The patient should remain in an upright position for 30 min after taking these medications to avoid pill-induced esophagitis.
Diagnosis
The National Osteoporosis Foundation (NOF) and the World Health Organization (WHO) recommend tests to determine bone mineral density, e.g., dual energy x-ray absroptiometry (DEXA scanning) in patients with specific diseases or conditions. The NOF recommends that all women over 65 and all men over 70 undergo testing. The NOF also recommends bone density testing for anyone over 50 who fractures a bone and for women of menopausal age who have risk factors (see Table "Risk Factors for Osteoporosis").
osteoporosis circumscripta cranii
osteoporosis of disuse
glucocorticoid osteoporosis
idiopathic juvenile osteoporosis
Juvenile osteoporosis.juvenile osteoporosis
post-traumatic osteoporosis
| Female |
| Advanced age |
| White or Asian |
| Thin, small-framed body |
| Positive family history |
| Low calcium intake |
| Early menopause (before age 45) |
| Sedentary lifestyle |
| Nulliparity |
| Smoking |
| Excessive alcohol or caffeine intake |
| High protein intake |
| High phosphate intake |
| Certain medications, when taken for a long time (e.g., aromatase inhibitors, glucocorticoid, phenytoin, proton pump inhibitors, selective serotonin reuptake inhibitors, thiazolidinediones, thyroid medication) |
| Endocrine diseases (hyperthyroidism, Cushing's disease, acromegaly, hypogonadism, hyperparathyroidism) |
| Diseases such as anorexia nervosa, autoimmune disorders, celiac disease, HIV/AIDS, multiple myeloma, multiple sclerosis, Parkinson disease, sickle cell disease |
os·te·o·po·rot·ic
(os'tē-ō-pŏr-ot'ik)Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp