Medical term:
paraplegia
paraplegia
[par″ah-ple´jah]impairment or loss of motor or sensory function in areas of the body served by the thoracic, lumbar, or sacral neurological segments owing to damage of neural elements in those parts of the spinal column. It spares the upper limbs but, depending on the level, may involve the trunk, pelvic organs, or lower limbs. This term is correctly used for describing cauda equina and conus medullaris injuries, but should not be used to refer to lumbosacral plexus lesions or injury to peripheral nerves outside the neural canal. adj., adj paraple´gic.
In the majority of cases, paraplegia results from disease or injury of the spinal cord that causes interference with nerve paths connecting the brain and the muscles. Conditions that may result in such interference include physical injuries, hemorrhage, tuberculosis, tumor, and syphilis. The loss of ability to use the legs may be accompanied by a loss of sensation in them and, in some cases, by loss of control over the bowel and bladder. Fortunately, much has been learned about the techniques of restoring paraplegics to normal activity, and today many are able to resume useful and productive lives.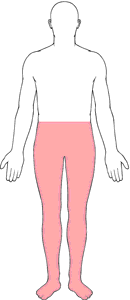
In the majority of cases, paraplegia results from disease or injury of the spinal cord that causes interference with nerve paths connecting the brain and the muscles. Conditions that may result in such interference include physical injuries, hemorrhage, tuberculosis, tumor, and syphilis. The loss of ability to use the legs may be accompanied by a loss of sensation in them and, in some cases, by loss of control over the bowel and bladder. Fortunately, much has been learned about the techniques of restoring paraplegics to normal activity, and today many are able to resume useful and productive lives.
Patient Care. Because rehabilitation is the ultimate goal for a paraplegic patient, the patient care during the early stages of the disorder must be particularly concerned with preventing complications that may stand in the way of successful rehabilitation. These complications include pressure ulcers, respiratory disorders, orthopedic deformities, urinary tract infections or calculi, and gastrointestinal disorders. The psychological and emotional aspects of paraplegia also must be considered. Many times the paraplegic patient is suddenly thrust into the role of dependence because of accidental injury to the spinal cord. This means that a tremendous adjustment to the condition must be made in a short time. Mental attitude and emotional response to paralysis will greatly affect the success of attempts at rehabilitation.
During the early stages of their illness patients may not be able to assist in their daily personal care, but as their condition improves and they are able to have more physical activity, they are encouraged to do as much as possible for themselves. As they learn to become less dependent on others, their attitude toward the future will improve. If it is anticipated that the patient will be confined to a wheelchair or will use crutches, transfer techniques for moving from bed to chair and from chair to other surfaces are taught. Wheelchairs and crutches are prescribed according to the individual patient's body build and weight, and the purpose for which they are to be used. The patient is instructed in correct crutch walking if crutches are to be used; if using a wheelchair, the patient is taught how to operate the chair to receive maximum benefit from it. Mastering these techniques can enhance mobility, increase independence, and give a degree of confidence that can greatly improve one's outlook.
During the early stages of their illness patients may not be able to assist in their daily personal care, but as their condition improves and they are able to have more physical activity, they are encouraged to do as much as possible for themselves. As they learn to become less dependent on others, their attitude toward the future will improve. If it is anticipated that the patient will be confined to a wheelchair or will use crutches, transfer techniques for moving from bed to chair and from chair to other surfaces are taught. Wheelchairs and crutches are prescribed according to the individual patient's body build and weight, and the purpose for which they are to be used. The patient is instructed in correct crutch walking if crutches are to be used; if using a wheelchair, the patient is taught how to operate the chair to receive maximum benefit from it. Mastering these techniques can enhance mobility, increase independence, and give a degree of confidence that can greatly improve one's outlook.
Care of the Skin. The type of bed used and the positioning of the patient with paraplegia will depend on the cause and extent of the paralysis and the preference of the health care provider. Patients with spinal cord injuries may be placed in traction or the spinal cord may be hyperextended by placing the patient's head at the foot of the bed and adjusting the bed. In some cases the health care provider may request a special orthopedic frame or specialized bed. These devices facilitate daily care but the patient still must be turned frequently (as allowed by the physician) and receive special skin care to avoid the development of pressure ulcers. Since these patients have no feeling below the point of damage to the spinal cord, they will not be aware of discomfort or other signs of pressure.
Respiratory Disorders. Hypostatic pneumonia and other respiratory problems are guarded against by deep breathing exercises. The patient should be protected from respiratory infections, such as the common cold, which can have serious complications in a paraplegic who is confined to bed.
Orthopedic Deformities. Until the patient is allowed out of bed and can engage in some form of physical activity, range of motion exercises for all joints should be performed frequently. Proper positioning of the feet and legs will help prevent contractures, footdrop, and ankylosis. A program of therapeutic exercise, including passive and active exercises, is initiated to maintain any remaining muscle function and to restore as much muscle activity in the affected parts as possible. If the patient is to use crutches or wheelchair he must strengthen his arm and shoulder muscles in preparation for transfer techniques. hydrotherapy and diathermy may be used to promote relaxation of muscle spasms and tension and to facilitate implementation of the exercise program.
Urinary Problems.urinary tract infections and the formation of calculi, particularly in the bladder, present real problems for the patient with paralysis. If there is no control over urination, an indwelling catheter may be the technique of choice for keeping the patient dry, but it also predisposes to infection. A thorough assessment of the patient's status and potential for achieving bladder control should be made before a final choice is made.
Ideally, the patient learns to achieve bladder control through an intensive bladder training program designed to fit individual needs. Whether this can be accomplished depends on the extent of nerve damage and the degree of success in avoiding such complications as infection and calculi. The achievement of bladder control is more difficult than bowel control. Patients with neurogenic bladder are unaware of the need to urinate and therefore require training to initiate urination. In some patients the bladder empties by reflex, and training involves techniques to make reflex emptying more effective. Intermittent catheterization may also be used. If the lesion causing paralysis is at the second, third, or fourth sacral segment, the bladder is flaccid and training must be aimed at avoiding overdistention and dribbling. Some may never be able to achieve bladder control to any appreciable degree, requiring the use of catheters, penile clamps, or other collecting devices. ureterostomy or ureteroileostomy may be required in some cases.
The formation of bladder stones results from incomplete emptying of the bladder, with pooling of urine and inadequate elimination of wastes. To minimize the formation of stones it is recommended that the patient receive between 2500 and 3000 ml of fluid every 24 hours. Medications are often needed to change the urinary pH. The high calcium content of milk also may foster stone formation, and carbonated drinks irritate the bladder. A wide variety of liquids can be most effective in avoiding the formation of stones.
Ideally, the patient learns to achieve bladder control through an intensive bladder training program designed to fit individual needs. Whether this can be accomplished depends on the extent of nerve damage and the degree of success in avoiding such complications as infection and calculi. The achievement of bladder control is more difficult than bowel control. Patients with neurogenic bladder are unaware of the need to urinate and therefore require training to initiate urination. In some patients the bladder empties by reflex, and training involves techniques to make reflex emptying more effective. Intermittent catheterization may also be used. If the lesion causing paralysis is at the second, third, or fourth sacral segment, the bladder is flaccid and training must be aimed at avoiding overdistention and dribbling. Some may never be able to achieve bladder control to any appreciable degree, requiring the use of catheters, penile clamps, or other collecting devices. ureterostomy or ureteroileostomy may be required in some cases.
The formation of bladder stones results from incomplete emptying of the bladder, with pooling of urine and inadequate elimination of wastes. To minimize the formation of stones it is recommended that the patient receive between 2500 and 3000 ml of fluid every 24 hours. Medications are often needed to change the urinary pH. The high calcium content of milk also may foster stone formation, and carbonated drinks irritate the bladder. A wide variety of liquids can be most effective in avoiding the formation of stones.
Gastrointestinal Complications. A flaccid bowel produces abdominal distention and predisposes the patient to fecal impaction. The patient may have fecal incontinence as well as frequent accumulations of flatus and fecal material in the lower intestine. Rehabilitation of the patient then requires working out some method of bowel control so that regularity of defecation can be accomplished.
As in bladder training, the program for bowel training is designed according to the individual needs of the patient and ability to work with those who are developing the program. It is essential that an assessment be made of the patient's status in regard to nerve damage and potential for rehabilitation. In addition, it is important to know about the patient's previous bowel habits in regard to frequency and time of day for a movement.
The training program also should include attention to fluid and food intake. The patient learns to avoid foods that produce diarrhea and flatus, and to rely upon a daily intake of fluids sufficient to insure soft, formed stools. Adequate physical exercise also is helpful in establishing regularity of defecation. Rectal suppositories and digital stimulation at regular intervals may be necessary to stimulate evacuation at a time convenient for the patient.
As in bladder training, the program for bowel training is designed according to the individual needs of the patient and ability to work with those who are developing the program. It is essential that an assessment be made of the patient's status in regard to nerve damage and potential for rehabilitation. In addition, it is important to know about the patient's previous bowel habits in regard to frequency and time of day for a movement.
The training program also should include attention to fluid and food intake. The patient learns to avoid foods that produce diarrhea and flatus, and to rely upon a daily intake of fluids sufficient to insure soft, formed stools. Adequate physical exercise also is helpful in establishing regularity of defecation. Rectal suppositories and digital stimulation at regular intervals may be necessary to stimulate evacuation at a time convenient for the patient.
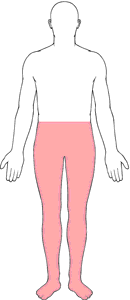
Paraplegia. From Frazier et al., 2000.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
par·a·ple·gi·a
(par'ă-plē'jē-ă),Paralysis of both lower extremities and, generally, the lower trunk.
[para- + plēgē, a stroke]
Farlex Partner Medical Dictionary © Farlex 2012
paraplegia
(păr′ə-plē′jə, -jē-ə)n.
Complete paralysis of the lower half of the body including both legs, usually caused by damage to the spinal cord.
par′a·ple′gic (-plē′jĭk) adj. & n.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
paraplegia
Neurology Complete paralysis, paresthesias, loss of sensation and control of voluntary movement in legs, post spinal cord injury or diseaseMcGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
par·a·ple·gi·a
(par'ă-plē'jē-ă)Paralysis of both lower extremities and, generally, the lower trunk.
[para- + plēgē, a stroke]
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
paraplegia
Paralysis of both lower limbs. Paraplegia caused by damage to the spinal cord is also associated with paralysis of the lower part of the trunk and loss of normal voluntary bladder and bowel control. In spastic paraplegia there is constant tension in the affected muscles often leading to fixed deformities. In flaccid paraplegia the muscles remain limp. Paraplegia may be hereditary or caused by birth injury, injury or disease of the brain or spinal cord or sometimes the peripheral nerves, as in alcoholic or dietary polyneuropathy, or by HYSTERIA or old age. See also PARAPARESIS.Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005
par·a·ple·gi·a
(par'ă-plē'jē-ă)Paralysis of both lower extremities and, generally, lower trunk.
[para- + plēgē, a stroke]
Medical Dictionary for the Dental Professions © Farlex 2012
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp