Medical term:
posture
posture
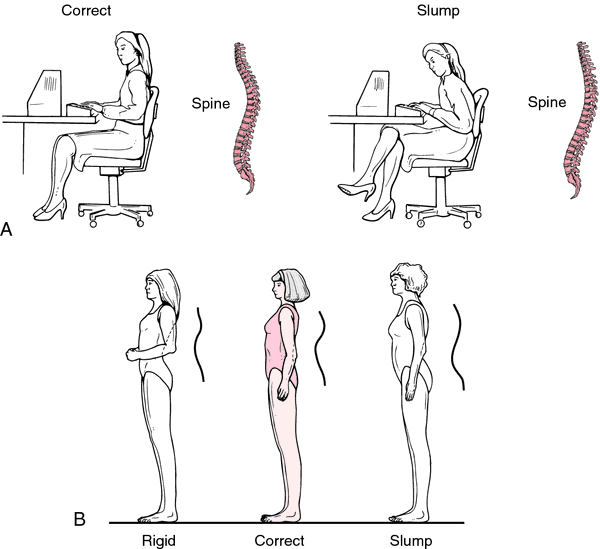
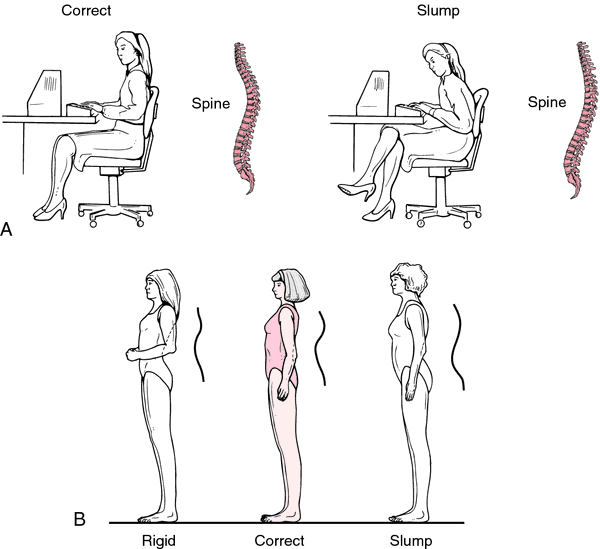
[pos´chur]Maintenance of good posture for a patient confined to bed or wheelchair is essential to the patient's general well-being and also is important in the prevention of deformities of the muscles and bones. The patient should be observed for evidence of “slumping,” in which the normal curves of the spine are exaggerated. The rib cage should be supported so that the ribs are elevated and there is no constriction of the chest wall. Pillows are arranged under the shoulders and head so that the chin is not forced downward on the chest. Excessive extension of the ankles should be avoided by adequate support against the soles of the feet. The legs should be supported so that the weight of one does not fall on the other. The arms are supported so that they do not lie across the chest or pull the shoulders into a rounded position. Frequent changing of position and adequate exercise of the limbs are also essential to the maintenance of good posture and the prevention of deformities.
calcium acetate
calcium carbonate
calcium chloride
calcium citrate
calcium gluconate
calcium lactate
tricalcium phosphate
Pharmacologic class: Mineral
Therapeutic class: Dietary supplement, electrolyte replacement agent
Pregnancy risk category C (calcium acetate, chloride, glubionate, gluceptate, phosphate), NR (calcium carbonate, citrate, gluconate, lactate)
Action
Increases serum calcium level through direct effects on bone, kidney, and GI tract. Decreases osteoclastic osteolysis by reducing mineral release and collagen breakdown in bone.
Availability
Calcium acetate-
Gelcaps: 667 mg
Tablets: 667 mg
Calcium carbonate-
Capsules: 1,250 mg
Lozenges: 600 mg
Oral suspension: 1,250 mg
Powder: 6.5 g
Tablets: 650 mg, 1,250 mg, 1,500 mg
Tablets (chewable): 750 mg, 1,000 mg, 1,250 mg
Tablets (gum): 300 mg, 450 mg, 500 mg
Calcium chloride-
Injection: 10% solution
Calcium citrate-
Tablets: 950 mg
Calcium gluceptate-
Injection: 22% solution
Calcium gluconate-
Injection: 10% solution
Tablets: 500 mg, 650 mg, 975 mg
Calcium lactate-
Tablets: 325 mg, 650 mg
Tricalcium phosphate-
Tablets: 600 mg
Indications and dosages
➣ Hypocalcemic emergency
Adults: 7 to 14 mEq I.V. of 10% calcium gluconate solution, 2% to 10% calcium chloride solution, or 22% calcium gluceptate solution
Children: 1 to 7 mEq calcium gluconate I.V.
Infants: Up to 1 mEq calcium gluconate I.V.
➣ Hypocalcemic tetany
Adults: 4.5 to 16 mEq calcium gluconate I.V., repeated as indicated until tetany is controlled
Children: 0.5 to 0.7 mEq/kg calcium gluconate I.V. three to four times daily as indicated until tetany is controlled
Neonates: 2.4 mEq/kg calcium gluconate I.V. daily in divided doses
➣ Cardiac arrest
Adults: 0.027 to 0.054 mEq/kg calcium chloride I.V., 4.5 to 6.3 mEq calcium gluceptate I.V., or 2.3 to 3.7 mEq calcium gluconate I.V.
Children: 0.27 mEq/kg calcium chloride I.V., repeated in 10 minutes if needed. Check calcium level before giving additional doses.
➣ Magnesium intoxication
Adults: Initially, 7 mEq I.V.; subsequent dosages based on patient response
➣ Exchange transfusions
Adults: 1.35 mEq calcium gluconate I.V. with each 100 ml of citrated blood
➣ Hyperphosphatemia in patients with end-stage renal disease
Adults: Two tablets P.O. daily, given in divided doses t.i.d. with meals. May increase gradually to bring serum phosphate level below 6 mg/dl, provided hypercalcemia doesn't develop.
➣ Dietary supplement
Adults: 500 mg to 2 g P.O. daily
Off-label uses
• Osteoporosis
Contraindications
• Hypersensitivity to drug
• Ventricular fibrillation
• Hypercalcemia and hypophosphatemia
• Cancer
• Renal calculi
• Pregnancy or breastfeeding
Precautions
Use cautiously in:
• renal insufficiency, pernicious anemia, heart disease, sarcoidosis, hyperparathyroidism, hypoparathyroidism
• history of renal calculi
• children.
Administration
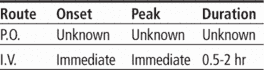
☞ When infusing I.V., don't exceed a rate of 200 mg/minute.
• Keep patient supine for 15 minutes after I.V. administration to prevent orthostatic hypotension.
• Administer P.O. doses 1 to 1½ hours after meals.
• Know that I.M. or subcutaneous administration is never recommended.
• Be aware that I.V. route is preferred in children.
• Be alert for extravasation, which causes tissue necrosis.
Adverse reactions
CNS: headache, weakness, dizziness, syncope, paresthesia
CV: mild blood pressure decrease, bradycardia, arrhythmias, cardiac arrest (with rapid I.V. injection)
GI: nausea, vomiting, diarrhea, constipation, epigastric pain or discomfort
GU: urinary frequency, renal calculi
Metabolic: hypercalcemia
Musculoskeletal: joint pain, back pain
Respiratory: dyspnea
Skin: rash
Other: altered or chalky taste, excessive thirst, allergic reactions (including facial flushing, swelling, tingling, tenderness in hands, and anaphylaxis)
Interactions
Drug-drug. Atenolol, fluoroquinolones, tetracycline: decreased bioavailability of these drugs
Calcium channel blockers: decreased calcium effects
Cardiac glycosides: increased risk of cardiac glycoside toxicity
Iron salts: decreased iron absorption
Sodium polystyrene sulfonate: metabolic alkalosis
Verapamil: reversal of verapamil effects
Drug-diagnostic tests. Calcium: increased level
Drug-food. Foods containing oxalic acid (such as spinach), phytic acid (such as whole grain cereal), or phosphorus (such as dairy products): interference with calcium absorption
Patient monitoring
• Monitor calcium levels frequently, especially in elderly patients.
Patient teaching
• Instruct patient to consume plenty of milk and dairy products during therapy.
• Refer patient to dietitian for help in meal planning and preparation.
• As appropriate, review all other significant and life-threatening adverse reactions and interactions, especially those related to the drugs, tests, and foods mentioned above.
pos·ture
(pos'tyūr, pos'cher),posture
(pŏs′chər)posture
Medtalk A position of the body. See Decerebrate posture, Decorticate posture, Fetal posture.pos·ture
(pos'chŭr)posture
(pos'chur) [Italian postura, fr. L. positura, fr. ponere, to place]coiled posture
decerebrate posture
decorticate posture
dorsal rigid posture
hyperlordotic posture
kyphosis-lordosis posture
modified plantigrade posture
open posture
orthopnea posture
orthotonos posture
prone posture
Prone.semireclining posture
slouched posture
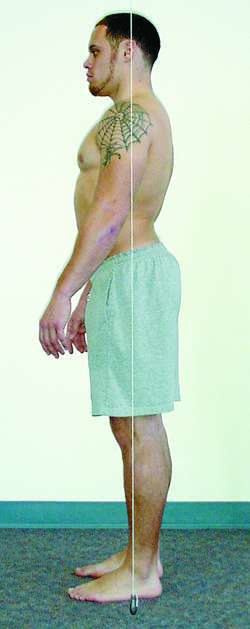
Swayback posture.standard posture
swayback posture
posture
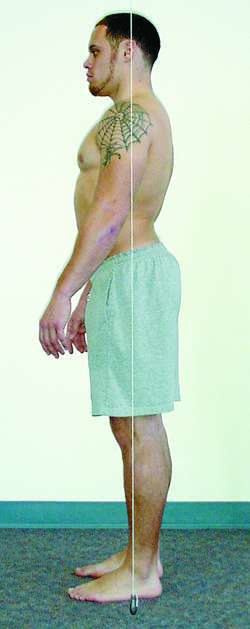
The relationship of different parts of the body to each other and to the vertical. In youth, posture is fully under voluntary control. Faulty posture tends to become permanent and may affect health as well as appearance.posture
[pos´chur]Maintenance of good posture for a patient confined to bed or wheelchair is essential to the patient's general well-being and also is important in the prevention of deformities of the muscles and bones. The patient should be observed for evidence of “slumping,” in which the normal curves of the spine are exaggerated. The rib cage should be supported so that the ribs are elevated and there is no constriction of the chest wall. Pillows are arranged under the shoulders and head so that the chin is not forced downward on the chest. Excessive extension of the ankles should be avoided by adequate support against the soles of the feet. The legs should be supported so that the weight of one does not fall on the other. The arms are supported so that they do not lie across the chest or pull the shoulders into a rounded position. Frequent changing of position and adequate exercise of the limbs are also essential to the maintenance of good posture and the prevention of deformities.
calcium acetate
calcium carbonate
calcium chloride
calcium citrate
calcium gluconate
calcium lactate
tricalcium phosphate
Pharmacologic class: Mineral
Therapeutic class: Dietary supplement, electrolyte replacement agent
Pregnancy risk category C (calcium acetate, chloride, glubionate, gluceptate, phosphate), NR (calcium carbonate, citrate, gluconate, lactate)
Action
Increases serum calcium level through direct effects on bone, kidney, and GI tract. Decreases osteoclastic osteolysis by reducing mineral release and collagen breakdown in bone.
Availability
Calcium acetate-
Gelcaps: 667 mg
Tablets: 667 mg
Calcium carbonate-
Capsules: 1,250 mg
Lozenges: 600 mg
Oral suspension: 1,250 mg
Powder: 6.5 g
Tablets: 650 mg, 1,250 mg, 1,500 mg
Tablets (chewable): 750 mg, 1,000 mg, 1,250 mg
Tablets (gum): 300 mg, 450 mg, 500 mg
Calcium chloride-
Injection: 10% solution
Calcium citrate-
Tablets: 950 mg
Calcium gluceptate-
Injection: 22% solution
Calcium gluconate-
Injection: 10% solution
Tablets: 500 mg, 650 mg, 975 mg
Calcium lactate-
Tablets: 325 mg, 650 mg
Tricalcium phosphate-
Tablets: 600 mg
Indications and dosages
➣ Hypocalcemic emergency
Adults: 7 to 14 mEq I.V. of 10% calcium gluconate solution, 2% to 10% calcium chloride solution, or 22% calcium gluceptate solution
Children: 1 to 7 mEq calcium gluconate I.V.
Infants: Up to 1 mEq calcium gluconate I.V.
➣ Hypocalcemic tetany
Adults: 4.5 to 16 mEq calcium gluconate I.V., repeated as indicated until tetany is controlled
Children: 0.5 to 0.7 mEq/kg calcium gluconate I.V. three to four times daily as indicated until tetany is controlled
Neonates: 2.4 mEq/kg calcium gluconate I.V. daily in divided doses
➣ Cardiac arrest
Adults: 0.027 to 0.054 mEq/kg calcium chloride I.V., 4.5 to 6.3 mEq calcium gluceptate I.V., or 2.3 to 3.7 mEq calcium gluconate I.V.
Children: 0.27 mEq/kg calcium chloride I.V., repeated in 10 minutes if needed. Check calcium level before giving additional doses.
➣ Magnesium intoxication
Adults: Initially, 7 mEq I.V.; subsequent dosages based on patient response
➣ Exchange transfusions
Adults: 1.35 mEq calcium gluconate I.V. with each 100 ml of citrated blood
➣ Hyperphosphatemia in patients with end-stage renal disease
Adults: Two tablets P.O. daily, given in divided doses t.i.d. with meals. May increase gradually to bring serum phosphate level below 6 mg/dl, provided hypercalcemia doesn't develop.
➣ Dietary supplement
Adults: 500 mg to 2 g P.O. daily
Off-label uses
• Osteoporosis
Contraindications
• Hypersensitivity to drug
• Ventricular fibrillation
• Hypercalcemia and hypophosphatemia
• Cancer
• Renal calculi
• Pregnancy or breastfeeding
Precautions
Use cautiously in:
• renal insufficiency, pernicious anemia, heart disease, sarcoidosis, hyperparathyroidism, hypoparathyroidism
• history of renal calculi
• children.
Administration
☞ When infusing I.V., don't exceed a rate of 200 mg/minute.
• Keep patient supine for 15 minutes after I.V. administration to prevent orthostatic hypotension.
• Administer P.O. doses 1 to 1½ hours after meals.
• Know that I.M. or subcutaneous administration is never recommended.
• Be aware that I.V. route is preferred in children.
• Be alert for extravasation, which causes tissue necrosis.
Adverse reactions
CNS: headache, weakness, dizziness, syncope, paresthesia
CV: mild blood pressure decrease, bradycardia, arrhythmias, cardiac arrest (with rapid I.V. injection)
GI: nausea, vomiting, diarrhea, constipation, epigastric pain or discomfort
GU: urinary frequency, renal calculi
Metabolic: hypercalcemia
Musculoskeletal: joint pain, back pain
Respiratory: dyspnea
Skin: rash
Other: altered or chalky taste, excessive thirst, allergic reactions (including facial flushing, swelling, tingling, tenderness in hands, and anaphylaxis)
Interactions
Drug-drug. Atenolol, fluoroquinolones, tetracycline: decreased bioavailability of these drugs
Calcium channel blockers: decreased calcium effects
Cardiac glycosides: increased risk of cardiac glycoside toxicity
Iron salts: decreased iron absorption
Sodium polystyrene sulfonate: metabolic alkalosis
Verapamil: reversal of verapamil effects
Drug-diagnostic tests. Calcium: increased level
Drug-food. Foods containing oxalic acid (such as spinach), phytic acid (such as whole grain cereal), or phosphorus (such as dairy products): interference with calcium absorption
Patient monitoring
• Monitor calcium levels frequently, especially in elderly patients.
Patient teaching
• Instruct patient to consume plenty of milk and dairy products during therapy.
• Refer patient to dietitian for help in meal planning and preparation.
• As appropriate, review all other significant and life-threatening adverse reactions and interactions, especially those related to the drugs, tests, and foods mentioned above.
pos·ture
(pos'tyūr, pos'cher),posture
(pŏs′chər)posture
Medtalk A position of the body. See Decerebrate posture, Decorticate posture, Fetal posture.pos·ture
(pos'chŭr)posture
(pos'chur) [Italian postura, fr. L. positura, fr. ponere, to place]coiled posture
decerebrate posture
decorticate posture
dorsal rigid posture
hyperlordotic posture
kyphosis-lordosis posture
modified plantigrade posture
open posture
orthopnea posture
orthotonos posture
prone posture
Prone.semireclining posture
slouched posture
Swayback posture.standard posture
swayback posture
posture
The relationship of different parts of the body to each other and to the vertical. In youth, posture is fully under voluntary control. Faulty posture tends to become permanent and may affect health as well as appearance.Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp