Medical term:
rheumatismal
rheumatic
[roo-mat´ik]pertaining to or affected with rheumatism.
rheumatic fever a disease associated with the presence of hemolytic streptococci in the body. It is called rheumatic fever because two common symptoms are fever and pain in the joints similar to that of rheumatism. It is relatively common, particularly in children between 5 and 15 years old; young adults in the early twenties are also susceptible.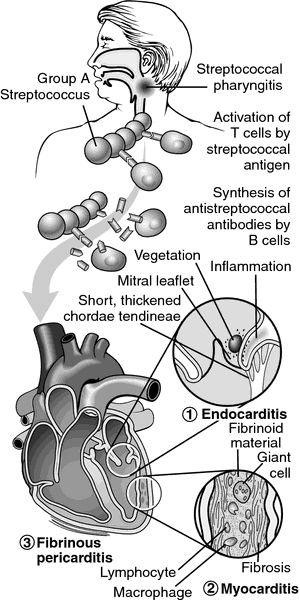
Causes. Rheumatic fever is a delayed sequela of an upper respiratory infection caused by the Group A hemolytic streptococcus that causes such common childhood illnesses as scarlet fever, tonsillitis, streptococcal sore throat (“strep throat”), and ear infections. It is only one of several complications that can result from a streptococcal infection.
The connection between rheumatic fever and a previous streptococcal infection has been proved only indirectly. In almost all cases of rheumatic fever there is evidence of previous streptococcal infection, and when the infection is treated promptly, the likelihood of rheumatic fever decreases sharply. There is evidence that the symptoms of rheumatic fever may result from an antigen-antibody reaction to one or more of the products of the hemolytic streptococcus, but the exact way this happens is not known. Rheumatic fever has been classified as an autoimmune disease. It tends to run in families, indicating a possible hereditary predisposition. Economic and environmental conditions such as a damp, cold climate and poor health habits may also be contributing factors.
The connection between rheumatic fever and a previous streptococcal infection has been proved only indirectly. In almost all cases of rheumatic fever there is evidence of previous streptococcal infection, and when the infection is treated promptly, the likelihood of rheumatic fever decreases sharply. There is evidence that the symptoms of rheumatic fever may result from an antigen-antibody reaction to one or more of the products of the hemolytic streptococcus, but the exact way this happens is not known. Rheumatic fever has been classified as an autoimmune disease. It tends to run in families, indicating a possible hereditary predisposition. Economic and environmental conditions such as a damp, cold climate and poor health habits may also be contributing factors.
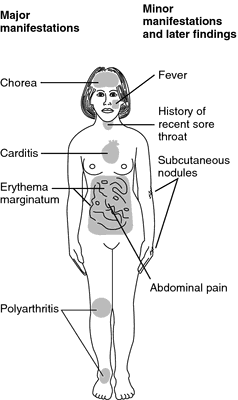
Symptoms. The initial symptoms usually appear 1 to 4 weeks after the streptococcal infection has occurred. The actual onset of the disease may be either gradual or sudden. The symptoms vary widely and may be of any degree of severity. The most common initial complaints are a slight fever, a feeling of tiredness, a vague feeling of pain in the limbs, and nosebleeds. If the disease takes an acute form, the fever may reach 40°C (104°F) by the second day and continue for several weeks, although the usual course of the fever is about 2 weeks. On the other hand, the fever may be quite mild.
Joint pain develops at any stage of the disease and lasts from a few hours to several weeks. The joints swell and are tender to the touch. The pain and swelling often subside in one group of joints and arise in another. As the pain subsides, the joints return to normal.
Other symptoms may include the spasmodic twitching movements known as sydenham's chorea, especially in girls between the ages of 6 and 11. A rash caused by the fever may appear upon the body. Nodules may be seen or felt under the skin at the elbow, knee, and wrist joints, and along the spine. Among the most serious signs is the development of a heart murmur and cardiac decompensation.
Joint pain develops at any stage of the disease and lasts from a few hours to several weeks. The joints swell and are tender to the touch. The pain and swelling often subside in one group of joints and arise in another. As the pain subsides, the joints return to normal.
Other symptoms may include the spasmodic twitching movements known as sydenham's chorea, especially in girls between the ages of 6 and 11. A rash caused by the fever may appear upon the body. Nodules may be seen or felt under the skin at the elbow, knee, and wrist joints, and along the spine. Among the most serious signs is the development of a heart murmur and cardiac decompensation.
Heart Damage. The seriousness of rheumatic fever lies primarily in the permanent damage it can do to the heart. The disease tends to recur, and the recurrent attacks may further weaken the heart. The usual cardiac complication is endocarditis (inflammation of the inner lining of the heart, including the membrane over the valves). As a valve heals, its edges may become so scarred and stiff that they fail to close properly. As a result, blood leaks through the valve when it is closed, producing the sound characteristic of a heart murmur. The valves may become thickened with scar tissue, so that the amount of blood that can flow through the heart is restricted. If there is severe stenosis of the mitral valve and the patient develops symptoms of congestive heart failure, surgery to enlarge the valve (mitral commissurotomy) may be indicated.
Treatment. The main purposes of treatment are reduction of fever and pain and promotion of the natural healing processes; no means have yet been discovered for fighting the disease directly. Until the introduction of antibiotics and steroids, the chief medications were aspirin and other salicylates. Penicillin is prescribed if there is evidence of an ongoing streptococcal infection or the chance of exposure to streptococcal infection. Prednisone may be prescribed to reduce the pain and swelling in the joints, but its effect on the ultimate course of the disease is controversial. If pain is severe, analgesic drugs may be given. Bed rest is an important part of the treatment, particularly if the disease has caused heart damage. Depending upon the severity of the disease, the patient may be kept in bed for months, and prolonged convalescence may be needed.
Patient Care. In the acute phase of rheumatic fever rest is most important to reduce the work load of the heart. The patient should be made as comfortable as possible and disturbed only when necessary. The care should be planned so that long periods of complete rest are possible. Proper positioning with adequate support of the limbs and maintenance of good body alignment is essential to rest and the prevention of complications.
The temperature, pulse, and respirations are checked and recorded at least every 4 hours during the day. The volume and rhythm as well as the rate of the pulse should be noted. The blood pressure is taken at least once a day. Fluid intake may be restricted if there is edema, and sodium intake may also be limited; in either case the reason for the restriction should be explained to the patient. A record is kept of the intake and output.
Frequent back care and good oral hygiene are needed to promote comfort and relaxation. When turning the patient, one should be gentle and slow, avoiding unnecessary handling of the joints, which may be tender and swollen.
During the convalescent period the patient is allowed a gradual return to physical activities. The amount of activity depends on the physician's orders and is based on the patient's pulse rate, erythrocyte sedimentation rate, and C-reaction protein test. Measures must be taken to avoid respiratory infections, which will retard the progress of the patient. Small, frequent feedings that provide a well-balanced diet are usually preferred to three meals a day, which may be only partially eaten by a patient who is not engaging in a normal amount of physical activity.
As the need for rest is decreased, some provision must be made for diversional activities that will help eliminate boredom and keep the child content. The psychologic effects of a prolonged period of enforced dependence on others must also be considered. The parents and the child will need encouragement and help in the transition from total dependence to relative independence. Parents and family members also will need support and guidance during adjustment to home care of the child. Referral to the public health nurse or home health care agency can help provide continuity of care and continued support.
The temperature, pulse, and respirations are checked and recorded at least every 4 hours during the day. The volume and rhythm as well as the rate of the pulse should be noted. The blood pressure is taken at least once a day. Fluid intake may be restricted if there is edema, and sodium intake may also be limited; in either case the reason for the restriction should be explained to the patient. A record is kept of the intake and output.
Frequent back care and good oral hygiene are needed to promote comfort and relaxation. When turning the patient, one should be gentle and slow, avoiding unnecessary handling of the joints, which may be tender and swollen.
During the convalescent period the patient is allowed a gradual return to physical activities. The amount of activity depends on the physician's orders and is based on the patient's pulse rate, erythrocyte sedimentation rate, and C-reaction protein test. Measures must be taken to avoid respiratory infections, which will retard the progress of the patient. Small, frequent feedings that provide a well-balanced diet are usually preferred to three meals a day, which may be only partially eaten by a patient who is not engaging in a normal amount of physical activity.
As the need for rest is decreased, some provision must be made for diversional activities that will help eliminate boredom and keep the child content. The psychologic effects of a prolonged period of enforced dependence on others must also be considered. The parents and the child will need encouragement and help in the transition from total dependence to relative independence. Parents and family members also will need support and guidance during adjustment to home care of the child. Referral to the public health nurse or home health care agency can help provide continuity of care and continued support.
Prevention. Preventive care is extremely important, especially when rheumatic fever has once occurred, since it tends to return unless precautionary steps are taken. The patient is given penicillin, orally every day or by intramuscular injection once a month, for many years in order to prevent streptococcal infection. A good nutritious diet and sufficient sleep are important. Administration of antibiotics to all patients with history of rheumatic fever undergoing even minor surgery, including tooth extraction, is important in preventing bacterial endocarditis. Prompt and effective treatment of “strep throat” among the general population has reduced the incidence of rheumatic fever.
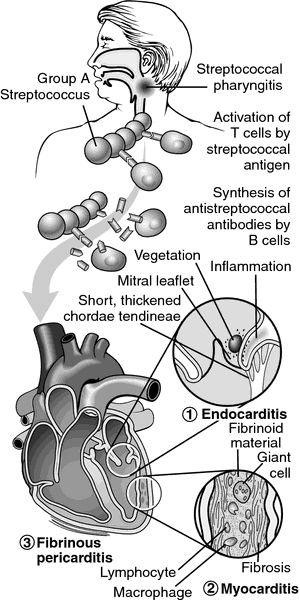
Pathogenesis of rheumatic fever. Following infection (“strep throat”), an immune response elicited by the streptococci acts on the heart and several other organs, most notably the joints, skin, and central nervous system. In the heart, it causes endocarditis, myocarditis, and pericarditis. From Damjanov, 2000.
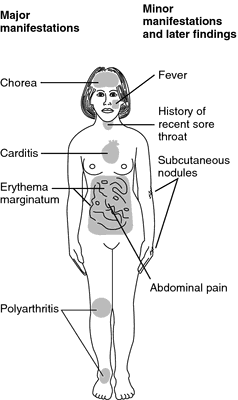
Manifestations of rheumatic fever. From Betz et al., 1994.
rheumatic heart disease the most important and constant manifestation of rheumatic fever, consisting of inflammatory changes with valvular deformities.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
rheu·mat·ic
(rū-mat'ik),Relating to or characterized by rheumatism.
Synonym(s): rheumatismal
[G. rheumatikos, subject to flux, fr. rheuma, flux]
Farlex Partner Medical Dictionary © Farlex 2012
rheumatic
(ro͞o-măt′ĭk)adj.
Of or relating to any of various diseases and disorders that chiefly affect the joints, tendons, ligaments, muscles, and bones and are characterized by pain, stiffness, and swelling. Rheumatoid arthritis, fibromyalgia, and gout are rheumatic diseases.
n.
1. One who is affected by a rheumatic disease or disorder.
2. rheumatics Informal Pains caused by a rheumatic disease or disorder.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
rheu·mat·ic
(rū-mat'ik)Relating to or characterized by rheumatism.
[G. rheumatikos, subject to flux, fr. rheuma, flux]
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp