Medical term:
Aller
leukemia
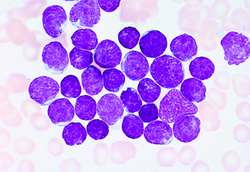
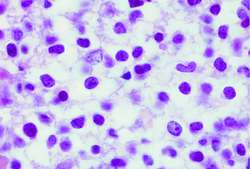
[loo-ke´me-ah]Acute leukemia is characterized by fatigue, headache, sore throat, and dyspnea, followed by symptoms of acute tonsillitis, stomatitis, bleeding from the mucous membranes of the mouth, alimentary canal, and rectum, and pain in the bones and joints. There eventually is enlargement of the lymph nodes, liver, and spleen. Common to all leukemias are the tendency to bleed and the resultant anemia and increased susceptibility to infection. The diagnosis of leukemia requires confirmation of leukemic cells in the bone marrow by bone marrow biopsy and aspiration. Abnormalities may also be seen in peripheral blood smears.
Because of the malignant nature of leukemia and the fear and anxiety created by the knowledge that one has a form of cancer, patients and their families and significant others will need help in coping with anxiety, mental depression, and realistic fears about dying and death. The financial burden of the illness and disruption of the life of the individual and the family also impose a special burden on them. Referral to appropriate persons and agencies that can help meet their needs is an essential part of the holistic care of the patient with leukemia.
ALL
ALL
acute lymphoblastic leukaemia
A malignant lymphoproliferative process, which commonly affects children and young adults, affecting ± 1800/year (US); ± 650/year (UK).Aetiology
ALL has a hereditary component; it is 20-fold increased in patients with Down syndrome; it is linked to benzene exposure, radiation therapy in ankylosing spondylitis.
Clinical findings
Abrupt onset, often ± 3-month history of fatigue, fever, haemorrhage from multiple sites, lymphadenopathy, hepatomegaly, splenomegaly.
Molecular pathology
Most are B cells and express CD19; 60% have karyotypic abnormalities; the most common cytogenetic abnormality is the cryptic t(12;21) translocation, resulting in TEL-AML fusion (25% of cases), followed by the t(1;19)(q23;p13.3) translocation, seen in 5% of cases.
Prognosis
90–95% achieve remission; improved cure rate is attributed to prophylaxis for meningeal leukaemia and more intense systemic chemotherapy. The current survival ranges from 20% to 75%.
FAB classification, acute leukaemias
Acute lymphocytic leukaemia (ALL)
L1—Small monotonous lymphocytes.
L2—Mixed L1- and L3-type lymphocytes.
L3—Large homogeneous blast cells.
ALL
ALL
leukemia
, leucemia (loo-ke'me-a) [ leuko- + -emia]Chronic leukemias, which have a relatively slow course, include chronic lymphocytic (CLL), chronic myelogenous or granulocytic (CML), and hairy cell leukemia (a subtype of CLL). Median survival in these illnesses is about 4 yr.
Acute leukemias include acute lymphocytic (ALL) and acute myeloid (myelogenous) (AML) leukemia. If untreated, these diseases are fatal within weeks or months. Each of these types of leukemia is discussed in subentries, below.
Etiology
All the different molecular events leading to the development of unchecked cellular reproduction in the leukemias result from genetic or chromosomal lesions in blood-forming cells. Duplications of genetic material (hyperdiploidy), loss of genetic information (hypodiploidy), inactivation of genes that normally suppress tumor development, chromosomal translocations, and the release of abnormal fusion proteins can all cause leukemia. These genetic lesions in turn can be produced by viruses, ionizing radiation, chemotherapeutic drugs, and toxic chemicals. Rarely, leukemias are caused by familial genetic syndromes (e.g., as ataxia telangiectasia, Bloom's syndrome, or Fanconi's syndrome).
Symptoms
Clinical findings such as anemia, fatigue, lethargy, fever, and bone and joint pain may be present. Physical findings include combinations of pallor, petechiae, or purpura; mucous membrane bleeding; enlarged liver, spleen, and kidneys; and tenderness over the sternum and other bones.
Diagnosis
Microscopic examination of peripheral blood and specimens of bone marrow are used to establish the diagnosis. These studies are followed by cytochemical and cytogenetic studies of abnormal cells found in the marrow or the peripheral blood to confirm the diagnosis with special stains and chromosomal analysis. Leukemic cells can also be identified by flow cytometry and immunocytochemistry, which rely on antibodies binding to and helping to identify malignant cells. The spread of leukemias to internal organs (e.g., the brain, the kidneys, or the lungs) may be evaluated with imaging tests (e.g., MRI studies, CT scans, or ultrasound).
Treatment
Chemotherapy, bone marrow transplantation, or both are used to treat leukemias. Regimens are devised regularly and are tailored to specific illnesses. Treatment is often given in several phases, with a period of induction chemotherapy to induce remission by completely eliminating leukemic cells from the bone marrow, followed by consolidation and maintenance phases. This multiphase treatment is designed to further deplete malignant cells from the bone marrow and to achieve complete cure.
Patient care
Patient care measures focus on eradicating the illness; managing complications; minimizing the effects of chemotherapy; preserving veins (often an indwelling port is inserted to administer chemotherapy); and providing comfort, education, and psychological support. The specific needs of patients (many of whom are children) and their families must be considered. Instruction is provided about drugs the patient will receive, including any adverse reactions and measures that will be taken to prevent or alleviate these effects. Prescribed chemotherapy is administered with special precautions when indicated for infusion and drug disposal. If the chemotherapy causes weight loss or anorexia, nutritional guidance is provided. Oral, skin, and rectal care must be meticulous, e.g., the nurse must thoroughly clean the skin before all invasive procedures, inspect the patient for perirectal erosions, use strict aseptic technique when starting an intravenous line, and change sets (i.e., intravenous tubing and associated equipment) according to chemotherapeutic protocols. Ports are irrigated according to agency protocol. If the patient is receiving intrathecal chemotherapy, the lumbar puncture site is checked frequently for bleeding or oozing. The patient and family are taught to recognize signs of infection (fevers, chills, sore throat, cough, urinary difficulties) and are urged to report these to the oncologist/hematologist promptly. To prevent infection in neutropenic patients, strict hand hygiene protocols, special diets, and (in hospitalized patients) laminar airflow or other reverse isolation measures are instituted. The patient is monitored for bleeding. If bleeding occurs, compresses are applied and the bleeding site is elevated. Transfusions of platelets and other blood cells are often needed. Complications associated with specific chemotherapeutic regimens (e.g., hair loss, nausea and vomiting, anemia, neutropenia, and low platelets) are explained to the patient, along with management strategies that will be employed. Prescribed analgesics are administered as needed, and noninvasive pain relief techniques and comfort measures (e.g., position changes, cutaneous stimulation, distraction, relaxation breathing, and imagery) may be used. Gentle oral hygiene measures and protective skin care are explained. Fluid intake should be increased to eliminate chemotherapy metabolites, and the patient advised to void more frequently to prevent cystitis. Dietary fiber is important, and stool softeners may be used to ensure normal bowel movements. Antidiarrheals usually control diarrhea, but the patient should be monitored for signs of dehydration. Fatigue is an anticipated adverse effect of treatment; therefore the patient is encouraged to alternate activity with rest periods and to obtain assistance with daily activities as necessary. Reproductive issues should be discussed with the patient. Patient care routines and visiting times should be flexible when hospitalization is required. The patient and family are encouraged to participate in care as much as possible. Referrals are made to social service agencies, home health care agencies, and support groups. If the patient does not respond to treatment and has reached the terminal phase of the disease, supportive nursing, palliative care, or hospice care should be discussed sensitively with patients and their caregivers.
acute lymphoblastic leukemia
acute lymphocytic leukemia
Abbreviation: ALLEtiology
Any of a wide range of acquired or congenital chromosomal abnormalities can cause ALL, including lesions that result in the release of excess growth factors from cells and those that cause the loss of cancer-suppressing genes.
Symptoms
Fatigue, lethargy, bleeding, bone and joint pain, and a predisposition to fever and infection are characteristic of ALL and other leukemias.
Diagnosis
The disease is suggested by the presence of abnormalities on the complete blood count or peripheral blood smear and is confirmed by immunophenotyping.
Treatment
In childhood, ALL induction chemotherapy often begins with steroids, vinca alkaloids, and asparaginase. This is followed, after bone marrow recovery, by consolidation chemotherapy with multidrug regimens, including high-dose methotrexate. Maintenance therapies, which may last 2 years or longer, include methotrexate, mercaptopurines, and other cytotoxic agents. Prophylaxis against central nervous system disease is accomplished by intrathecal drug administration. In referral hospitals, allogeneic stem cell transplantation is sometimes used for refractory disease. About 90% of treated children achieve remission. The 5-year survival of children with ALL is about 85%. Adult ALL is much less responsive to therapy; only about a third of adult patients are cured. In both childhood and adult ALL, allopurinol and hydration precede induction chemotherapy to prevent hyperuricemia caused by tumor lysis.
Prognosis
Late complications of therapy are not uncommon.
acute myelogenous leukemia
Abbreviation: AMLacute myeloid leukemia
Abbreviation: AMLAll forms of AML are marked by neoplastic replacement of normal bone marrow and circulation of immature cells (“blasts”) in the peripheral blood. Anemia and thrombocytopenia commonly occur. The central nervous system and other organs are occasionally invaded. Complete remissions occur in approximately 65% of treated patients; responses to treatment lasting 5 years are achieved in 15% to 25% of treated patients. Synonym: acute myelogenous l.; acute nonlymphocytic l.
Etiology
Genetic and chromosomal aberrations, such as are found in other leukemias, are characteristic.
Symptoms
Exertional fatigue as a result of anemia, bleeding due to thrombocytopenia, and infections due to a lack of normal white blood cells are common.
Treatment
Cytotoxic chemotherapies, with an induction phase followed by consolidation, are used. Typically, cytosine arabinoside and an anthracycline are used during induction for AML. Allogeneic bone marrow transplantation is used when a matching donor is available; stem cell transplantation is an option for some patients with specific cytogenetic abnormalities.
acute nonlymphocytic leukemia
Abbreviation: ANLLaleukemic leukemia
Leukemia cutis.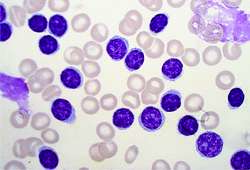
chronic lymphocytic leukemia
Abbreviation: CLLTreatment
Patients with advanced stages of the illness are often treated with chlorambucil, fludarabine, or other cytotoxic agents, often with rituximab (a monoclonal antibody) added to enhance response. Patients with early-stage disease are not usually given therapy.
chronic myelogenous leukemia
Abbreviation: CMLchronic myeloid leukemia
Abbreviation: CMLEtiology
CML results from a translocation of genetic material between chromosomes 9 and 22. The translocation results in the production of an abnormal tyrosine kinase that makes affected cells immortal.
Symptoms
CML often is diagnosed in asymptomatic patients who are found to have an unexplained leukocytosis when their complete blood counts are checked. Subsequent evaluation, including bone marrow aspiration and biopsy with cytogenetic analysis, reveal the Philadelphia chromosome.
Treatment
Imatinib mesylate (a drug that blocks an abnormal kinase made by Philadelphia chromosome positive CML cells) effectively reduces the number of tumor cells in the chronic phase of CML to normal in nearly 90% of patients. An alternative is stem cell transplantation.
leukemia cutis

hairy cell leukemia
Abbreviation: HCLSymptoms
Weight loss, hypermetabolism, infectious complications, and abdominal discomfort due to splenic enlargement are common.
Treatment
Cladribine, pentostatin, interferon alfa, and rituximab (a monoclonal antibody) are representative chemotherapeutic options.
mixed-lineage leukemia
Abbreviation: MLL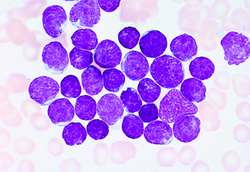
acute lymphocytic leukemia
Abbreviation: ALLEtiology
Any of a wide range of acquired or congenital chromosomal abnormalities can cause ALL, including lesions that result in the release of excess growth factors from cells and those that cause the loss of cancer-suppressing genes.
Symptoms
Fatigue, lethargy, bleeding, bone and joint pain, and a predisposition to fever and infection are characteristic of ALL and other leukemias.
Diagnosis
The disease is suggested by the presence of abnormalities on the complete blood count or peripheral blood smear and is confirmed by immunophenotyping.
Treatment
In childhood, ALL induction chemotherapy often begins with steroids, vinca alkaloids, and asparaginase. This is followed, after bone marrow recovery, by consolidation chemotherapy with multidrug regimens, including high-dose methotrexate. Maintenance therapies, which may last 2 years or longer, include methotrexate, mercaptopurines, and other cytotoxic agents. Prophylaxis against central nervous system disease is accomplished by intrathecal drug administration. In referral hospitals, allogeneic stem cell transplantation is sometimes used for refractory disease. About 90% of treated children achieve remission. The 5-year survival of children with ALL is about 85%. Adult ALL is much less responsive to therapy; only about a third of adult patients are cured. In both childhood and adult ALL, allopurinol and hydration precede induction chemotherapy to prevent hyperuricemia caused by tumor lysis.
Prognosis
Late complications of therapy are not uncommon.
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp