Medical term:
Flonase
fluticasone propionate
fluticasone furoate
Pharmacologic class: Corticosteroid
Therapeutic class: Respiratory inhalant (Flovent, Flonase), anti-inflammatory drug (Cutivate)
Pregnancy risk category C
Action
Unknown. Has potent vasoconstrictive and anti-inflammatory properties.
Availability
fluticasone propionate
Inhalation aerosol, metered (Flovent HFA): 44 mcg, 110 mcg, 220 mcg
Inhalation powder, metered (Flovent Diskus): 50 mcg, 100 mcg, 250 mcg
Nasal spray (Flonase): 50 mcg
Topical cream (Cutivate): 0.005%
Topical ointment (Cutivate): 0.005%
fluticasone furoate
Nasal spray (Veramyst): 27.5 mcg fluticasone furoate in each 50-microliter spray in 10-g bottle containing 120 sprays
Indications and dosages
➣ Prophylaxis of asthma and treatment of asthma for patients requiring oral corticosteroid therapy (Flovent HFA and Flovent Diskus)
Adults and children age 4 and older: Recommended starting dosage and highest recommended dosage, based on prior asthma therapy, are listed in charts below.
Recommended Flovent FHA dosages
For Adults and adolescents age 12 and older
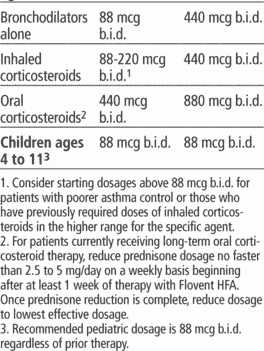
Recommended Flovent Diskus dosages


➣ Seasonal and perennial allergic and nonallergic rhinitis (Flonase)
Adults: Two sprays in each nostril daily or one spray in each nostril b.i.d. After first few days, may reduce dosage to one spray in each nostril daily; some patients may find p.r.n. use of two sprays in each nostril daily effective for symptom control. Maximum dosage is 200 mcg daily (two sprays in each nostril).
Adolescents and children ages 4 and older: Initially, one spray in each nostril daily. If patient doesn't respond, may increase to two sprays in each nostril. Once adequate control is achieved, reduce dosage to one spray in each nostril daily.
➣ Symptoms of seasonal and perennial allergic rhinitis (Veramyst)
Adults and adolescents age 12 and older: 110 mcg (2 sprays per nostril) once daily
Children ages 2 to 11: 55 mcg (1 spray per nostril) once daily
➣ Inflammatory and pruritic manifestations of corticosteroid-responsive atopic dermatoses
Adults and children ages 3 months and older: Apply thin film of Cutivate cream to affected skin area once or twice daily.
➣ Other corticosteroid-responsive dermatoses
Adults and children ages 3 months and older: Apply thin film of Cutivate cream to affected skin area b.i.d.
Contraindications
• Hypersensitivity to drug or its components
• Primary treatment of status asthmaticus or other acute asthma episodes necessitating intensive measures (Flovent FHA, Flovent Diskus)
• Severe allergy to milk proteins (Flovent Diskus)
Precautions
Use cautiously in:
• recurrent epistaxis, recent nasal septal ulcer, nasal surgery, or trauma
• severe hepatic disease (Veramyst)
• glaucoma and cataracts
• tuberculosis; respiratory tract infection; fungal, bacterial, viral, or parasitic infections; ocular herpes simplex
• hypercorticism and adrenal suppression (when used at higher than recommended dosages or in susceptible persons)
• concurrent use of other CYP3A inhibitors (such as ketoconazole; use not recommended with ritonavir)
• Candida albicans infection (Flovent, Veramyst)
• elderly patients (Flonase, Veramyst)
• pregnant or breastfeeding patients (Flovent, Flonase, Veramyst)
• children younger age than 4 (Flonase, Flovent)
• children younger than age 2 (Veramyst).
Administration
• Know that Flonase may cause immediate hypersensitivity reaction (contact dermatitis).
• Be aware that topical ointment should be used in adults only.
• Prime Veramyst nasal spray before first use, when not used for more than 30 days, or if cap has been left off bottle for 5 days or more.
• Administer inhalation powder by oral inhalation only.

Adverse reactions
CNS: Cutivate ointment-lightheadedness; Flonase-headache, dizziness; Flovent-headache, dizziness, giddiness; Veramyst-headache
EENT: Flonase-cataract, glaucoma, increased intraocular pressure, epistaxis, nasal burning or irritation, bloody nasal mucus, runny nose, pharyngitis; Flovent-cataract, glaucoma, nasal congestion, nasal septum perforation, nasal discharge, nasal sinus pain, sinusitis, rhinitis, allergic rhinitis, pharyngitis, dysphonia; Veramyst-cataract, glaucoma, increased intraocular pressure, epistaxis, pharyngolaryngeal pain, nasal ulceration
GI: Flonase-nausea, vomiting, diarrhea, abdominal pain; Flovent-nausea, vomiting, diarrhea, dyspepsia, stomach disorder, oral candidiasis
GU: Flovent-dysmenorrhea
Metabolic: Flovent, Veramyst-hypercorticism and adrenal suppression
Musculoskeletal: Flonase-aches and pains; Flovent-joint pain, limb pain, sprain, strain, aches and pains, reduced bone mineral density; Veramyst-back pain
Respiratory: Flonase-asthma symptoms, cough, bronchitis, wheezing (rare); Flovent-upper respiratory tract infection, influenza, bronchitis, chest congestion, bronchospasm; Veramyst-cough
Skin: Cutivate cream-pruritus, skin dryness, skin burning, erythematous rash, dusky erythema, eczema exacerbation, skin irritation, urticaria; Cutivate ointment-skin burning or irritation, hypertrichosis, increased erythema, hives; Flovent-urticaria, rash, skin eruption
Other: Cutivate cream or ointment-numbness of fingers, facial or nonfacial telangiectasia; Flonase-fever, flulike symptoms, hypersensitivity reaction; Flovent-dental problems, fever, C. albicans infection, immunosuppression, immediate or delayed hypersensitivity reactions, angioedema; anaphylaxis; Veramyst-pyrexia
Interactions
Drug-drug. Ketoconazole, other strong CYP3A inhibitors: increased fluticasone exposure (with Flonase, Flovent, Veramyst)
Ritonavir: increased systemic corticosteroid effects (with Flonase, Flovent, Veramyst)
Drug-diagnostic tests. Adrenocorticotropic hormone stimulation test, plasma cortisol test, urinary free cortisol test: interference with test results
Patient monitoring
☞ Monitor patient for withdrawal symptoms after Flovent is discontinued.
• Stay alert for systemic corticosteroid effects when administering Flovent, Flonase, or Veramyst.
• Observe for reduced growth rate in child or adolescent using Flovent, Flonase, or Veramyst.
• When giving Flovent, watch for eosinophilic conditions, such as Churg-Strauss syndrome.
☞ When giving Flonase, assess for epistaxis, wheezing, nasal septum perforation, cataracts, glaucoma, and increased intraocular pressure (rare reaction).
☞ When giving Veramyst, assess for epistaxis, nasal septum perforation, cataracts, glaucoma, and increased intraocular pressure (rare reaction).
Patient teaching
• Tell patient to take drug exactly as prescribed.
• Teach patient proper use of prescribed form.
☞ Advise patient to immediately report signs of allergic reaction.
• Caution patient to avoid exposure to people with chickenpox or measles.
• Advise female patient taking Flonase, Flovent, or Veramyst to inform prescriber if she is pregnant or breastfeeding.
• As appropriate, review all other significant and life-threatening adverse reactions and interactions, especially those related to the drugs and tests mentioned above.
fluticasone (nasal)
(floo-ti-ka-sone) ,Avamys
(trade name),Flonase
(trade name),Veramyst
(trade name)Classification
Therapeutic: anti inflammatories steroidalPharmacologic: corticosteroids
Indications
Action
Therapeutic effects
Pharmacokinetics
Time/action profile (improvement in symptoms)
| ROUTE | ONSET | PEAK | DURATION |
| Intranasal | few days | up to 3 wk | unknown |
Contraindications/Precautions
Adverse Reactions/Side Effects
Central nervous system
- headache
Ear, Eye, Nose, Throat
- epistaxis
- nasal burning
- nasal irritation
- nasopharyngeal fungal infection
- pharyngitis
Gastrointestinal
- nausea
- vomiting
Endocrinologic
- adrenal suppression (↑ dose, long-term therapy only)
- ↓ growth (children)
Dermatologic
- rash
- urticaria
Respiratory
- cough
Miscellaneous
- anaphylaxis
- angioedema
Interactions
Drug-Drug interaction
Ritonavir and ketoconazole ↓ metabolism and ↑ levels of fluticasone. Concomitant use of ritonavir and fluticasone not recommended.Route/Dosage
Availability (generic available)
Nursing implications
Nursing assessment
- Monitor degree of nasal stuffiness, amount and color of nasal discharge, and frequency of sneezing.
- Patients on long-term therapy should have periodic otolaryngologic examinations to monitor nasal mucosa and passages for infection or ulceration.
- Monitor growth rate in children receiving chronic therapy; use lowest possible dose.
- Monitor for signs and symptoms of hypersensitivity reactions (rash, pruritis, swelling of face and neck, dyspnea) periodically during therapy.
- Lab Test Considerations: Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitary-adrenal (HPA) axis suppression in chronic therapy. Children and patients using higher than recommended doses are at highest risk for HPA suppression.
Potential Nursing Diagnoses
Ineffective airway clearance (Indications)Risk for infection (Side Effects)
Deficient knowledge, related to medication regimen (Patient/Family Teaching)
Implementation
- Do not confuse Flovent (fluticasone oral inhalation) with Flonase (fluticasone nasal spray).
- After the desired clinical effect has been obtained, attempts should be made to decrease dose to lowest amount. Gradually decrease dose every 2–4 wk as long as desired effect is maintained. If symptoms return, dose may briefly return to starting dose.
- Intranasal: Patients also using a nasal decongestant should be given decongestant 5–15 min before corticosteroid nasal spray. If patient is unable to breathe freely through nasal passages, instruct patient to blow nose gently in advance of medication administration.
Patient/Family Teaching
- Advise patient to take medication exactly as directed. Take missed doses as soon as remembered unless almost time for next dose.
- Instruct patient in correct technique for administering nasal spray (see ). Shake well before use. Before first-time use, prime unit by spraying 6 times. If not used for at least 7 days or if cap left off for more than 5 days, reprime unit. Warn patient that temporary nasal stinging may occur.
- Instruct patient to stop fluticasone and notify health care professional immediately if signs of anaphylaxis (rash, hives, difficulty breathing, swollen lips or throat) occur.
- Instruct patient to notify health care professional of all Rx or OTC medications, vitamins, or herbal products being taken and consult health care professional before taking other Rx, OTC, or herbal products.
- Advise female patients to notify health care professional if pregnancy is planned or suspected or if breastfeeding.
- Instruct patient to notify health care professional if symptoms do not improve within 1 mo or if symptoms worsen.
Evaluation/Desired Outcomes
- Resolution of nasal stuffiness, discharge, and sneezing in seasonal or perennial rhinitis.
Flonase
(flō′nāz′)Flonase™
Fluticasone propionate, see there.Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp