Medical term:
cardioversion
Cardioversion
Definition
Purpose
Precautions
Description
Preparation
Aftercare
Risks
Normal results
Key terms
Resources
Organizations
cardioversion
[kahr´de-o-ver″zhun]Cardioversion is most effective in terminating arrhythmias due to continuous reentry, including atrial flutter, atrial fibrillation, paroxysmal supraventricular tachycardia, ventricular tachycardia, and ventricular fibrillation. Patients who have had a recent myocardial infarction and resultant atrial, nodal, or ventricular tachycardia are the most frequent candidates for cardioversion. Those with severe, longstanding arrhythmias due to chronic extensive heart disease usually do not benefit from this procedure.
Cardioversion should be done only by trained physicians in a setting where resuscitation equipment and respiratory support are readily at hand. Serum potassium levels must be within normal limits at the time of procedure because hypokalemia increases the patient's chance of developing deadly postconversion dysrhythmias. If necessary, potassium salts can be given prior to the procedure. digitalis toxicity predisposes the patient to life-threatening dysrhythmiasduring cardioversion and the drug should be withheld several days prior to the anticipated procedure. hypoxia and acidosis may decrease the chances of successful cardioversion.
car·di·o·ver·sion
(kar'dē-ō-ver'zhŭn),cardioversion
(kär′dē-ō-vûr′zhən)cardioversion
Interventional cardiology The conversion of a cardiac arrhythmia, usually a tachyarrhythmia to a normal sinus rhythm; CV is most effective in terminating tachycardias due to defective reentry–eg, atrial flutter, A Fib, AV nodal entry, WPW syndrome, V tach with a pulse, flutter; the electric shock depolarizes all excitable myocardium, prolongs refractoriness, interrupts reentry circuits, and establishes electrical homogeneity; it is attempted in Pts with AFib in order to improve cardiac function, relieve symptoms, and ↓ risk of thrombus formation; transesophageal echocardiography identifies Pts with atrial emboli requiring short-term anticoagulation with heparin before cardioversion. See Chemical cardioversion, Direct current cardioversion, Single-pulse cardioversion. Cf Defibrillation.car·di·o·ver·sion
(kahr'dē-ō-vĕr'zhŭn)cardioversion
(kar'de-o-ver?zhun) [? + L. versio, a turning]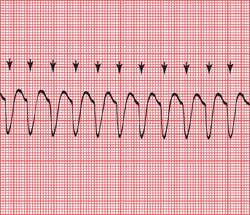
CAUTION!
Electrical cardioversion should not be used in patients who have recently eaten (because of the risk of regurgitation of stomach contents), in patients with severe electrolyte abnormalities, in patients with some drug overdoses, or in patients unable or unwilling to give informed consent. Patients need to be advised of the risks of cardioversion, including the rare precipitation of ventricular fibrillation and ventricular tachycardia, the development of bradyarrhythmias or heart blocks, and the possibility of embolic stroke.Patient care
The procedure, expected sensations, complications, and risks are explained to and clarified for the patient. Emotional support is provided throughout the procedure and at its conclusion. The patient's medication history is reviewed, and cardiac glycoside use is reported to the health care provider, along with the patient's electrolyte levels. Emergency equipment (including ACLS drugs, a bag mask device, supplemental oxygen, suction, laryngoscope and appropriate size ET tube, defibrillator, and supplies for intravenous injection) are assembled at the bedside. In the hospital setting, emergency personnel (respiratory technicians, anesthesiologists, nurses, and paramedics) may assist the attending physician. The patient's vital signs are checked, an intravenous infusion is started, and the patient is connected to a continuous ECG monitor. Dentures are removed from the mouth, and necklaces or pendants, as well as nitroglycerin patches, are removed from the chest and neck. Chest electrodes are placed to facilitate recording of tall R waves without interfering with paddle placement. A 12-lead ECG is obtained and the patient is given enriched oxygen to breathe. The patient is placed in a supine position, and adequate ventilation and oxygenation are ensured by observation and oximetry. A sedative, such as diazepam, is provided as prescribed unless the patient is profoundly hypotensive. The defibrillator leads are attached to the patient. The cardioverter/defibrillator is set to synchronize with the patient's QRS complex, and the recording is checked to ensure that each R wave is marked. The control is set to the energy level prescribed by the health care provider or by protocol. The defibrillation pads for hands-free operation (or manual paddles) are placed in prescribed positions on the chest wall. All personnel in attendance are cleared from direct contact with the patient or his or her bed. After this is carefully verified, the electrical current is discharged. The monitor is immediately analyzed to ensure that the dysrhythmia has resolved. If it has not, the procedure is repeated, usually with a higher energy setting. After successful cardioversion, health care personnel monitor the posttreatment rhythm and vital signs until the patient's stability is assured. The patient's skin is inspected for burns. See: defibrillation
cardioversion
The convertion of a dangerously rapid or irregular heart beat to normal rhythm with an electric shock. A common use is in defibrillation for one of the forms of CARDIAC ARREST or in the correction of ATRIAL FIBRILLATION.Patient discussion about cardioversion
Q. Does anyone know if its possible to get breast implants if i have an implanted defibrillator? I have hypertrophic cardiomyopathy. I'm 27 and in great health, I workout 6 days a week and I have no further symptoms.
Ince again,
Thanks!
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp