Medical term:
cataract
cataract
[kat´ah-rakt]Blurred and dimmed vision are often the first symptoms. The patient may find that a brighter reading light is needed, or objects must be held closer to the eyes for better vision. Continued clouding of the lens may cause double vision; eventually there may be a need for frequent changes of eyeglasses. These symptoms do not necessarily indicate cataract, but if any of them are present, an ophthalmologist should be consulted immediately.
The lens of the eye serves only to focus light rays upon the retina. After cataract extraction the loss of the natural lens is compensated for by either special eyeglasses or contact lenses. Implantation of a permanent artificial lens, either during cataract surgery or later, is an alternative to use of cataract spectacles and a removable contact lens.
cat·a·ract
(kat'ă-rakt), Avoid the redundant phrase ocular cataract.cataract
(kăt′ə-răkt′)cataract
Lens opacity Ophthalmology Partial or complete opacification of the ocular lens or capsule, which impairs vision or causes blindness Classification Morphology–size, shape, location; etiology–eg DM, corticosteroids, trauma, und so weiter; time of occurrence–eg in elderly Clinical Double or blurred vision; ↑ sensitivity to light, glare Diagnosis Slit lamp microscopy Treatment Phacoemulsion, surgery. See Black cataract, Congenital cataract, Snowflake cataract, Sunflower cataract.cat·a·ract
(kat'ăr-akt)cataract
(kat'a-rakt?) [L. catar(r)acta, fr Gr. katarraktes, waterfall]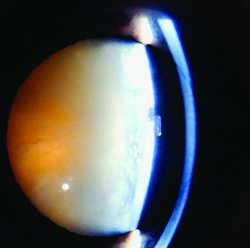
Symptoms
At first, vision is distorted, particularly during night driving or in very bright light, causing light sensitivity (photophobia). As the cataract progresses, severe visual impairment develops.
Prevalence
Ninety percent of adults over 65 have cataracts.
Treatment
Removal of the lens is the only effective treatment. In the U.S. about a million cataract surgeries are performed annually, usually as an outpatient, same-day procedure. Typically, the lens and its anterior capsule are removed by extracapsular extraction or by phacoemulsification, leaving the posterior capsule of the lens in place, and a posterior chamber intraocular lens is inserted where the patient’s own lens used to be. See: extracapsular extraction; intraocular lens; phacoemulsification
Patient care
Preoperative: The procedure is explained to the patient. An antiseptic facial scrub is performed. Mydriatic and cycloplegic eye drops are instilled to dilate the pupil, followed by lidocaine jelly and betadine drops prior to surgery; osmotic diuretics may be given to reduce intraocular pressure. An intravenous access is initiated, and antibiotics, a sedative, short-acting general anesthetic, and a local anesthetic are provided.
Postoperative: The patient is instructed to wear a clear eyeshield if prescribed, and to call if experiencing pain, or loss of vision. Blurred vision the day of surgery is to be expected. Eye drops are to be placed as directed and the patient should not swim or strain himself. A postoperative checkup visit is scheduled for the day following surgery. Both patient and family are taught how to inspect the eye for redness or watering and to report these conditions as well as any photophobia or sudden visual changes; wash hands well and then to instill eye drops (antibiotic to prevent inflammation and steroids to reduce infection) as prescribed; and to maintain the eye patch and shield as prescribed by the surgeon. The patient should be taught to protect the eye from bright sunlight or glare by wearing dark glasses. The patient should not swim or strain himself or herself.
capsular cataract
cortical cataract
hypermature cataract
immature cataract
lenticular cataract
mature cataract
morgagnian cataract
See: Morgagni cataractnuclear cataract
, nuclear sclerotic c.posterior cortical cataract
Posterior subcapsular cataract.posterior subcortical cataract
Posterior subcapsular cataract.posterior subcapsular cataract
Abbreviation: PSCradiation cataract
senile cataract
zonular cataract
cataract
Opacification of the internal focusing lens of the eye (the crystalline lens) due to changes in hydration and denaturation of protein causing irreversible structural changes in the orderly arrangement of the fibres from which the lens is made. There may also be aggregation of crystallin protein in the lens. These changes may be CONGENITAL, the result of trauma, or, most commonly, an apparently spontaneous age-related effect. Some experts believe that age-related cataract is caused by ultraviolet radiation in sunlight but others disagree.Cataract
cataract
age-related cataract Cataract affecting older persons. It is the most common type of cataract and may take several forms: cortical, cuneiform, nuclear, mature or subcapsular. Syn. senile cataract.
anterior capsular cataract A small central opacity located on the anterior lens capsule, either of congenital origin or due to a perforating ulcer of the cornea. See Vogt's sign.
axial cataract An opacity situated along the anteroposterior axis of the crystalline lens (Fig. C3).
bipolar cataract An opacity involving both the anterior and the posterior poles of the lens (Fig. C3). See polar cataract.
blue cataract See blue-dot cataract.
blue-dot cataract A developmental anomaly of the crystalline lens characterized by numerous small opacities in the outer nucleus and cortex, which appear as translucent bluish dots. The condition is very common and does not usually affect acuity. Syn. blue cataract; diffuse cataract; punctate cataract.
brown; brunescent cataract See nuclear cataract.
capsular cataract An opacity confined only to the capsule of the crystalline lens, anteriorly or posteriorly. It is usually congenital, although it may be acquired as a result of trauma or inflammation.
central cataract See nuclear cataract.
chalky cataract A cataract characterized by the presence of lime salt deposits.
Christmas tree cataract A rare type of diffuse age-related cataract in which the opacities appear as highly reflective crystals.
complicated cataract A cataract caused by or accompanying another intraocular disease, such as glaucoma, cyclitis, anterior uveitis or a hereditary retinal disorder such as retinitis pigmentosa or Leber's disease. Syn. secondary cataract. See cuneiform cataract; Leber's hereditary optic atrophy; retinitis pigmentosa; Down's syndrome; Fuchs' syndrome; rubella syndrome.
congenital cataract Cataract occurring as a result of faults in the early development of the lens. Some may be hereditary, usually autosomal dominant. The cause of others may be chromosomal abnormalities (e.g. Down's syndrome, Turner's syndrome), carbohydrate metabolic disorders (galactosaemia, galactokinase deficiency), rubella syndrome, etc. The condition requires urgent treatment to prevent the development of amblyopia. See capsular cataract; lamellar cataract; nuclear cataract; polar cataract; sutural cataract.
coronary cataract A cataract characterized by a series of opacities having the shape of a crown or ring near the periphery of the lens (Fig. C3).
cortical cataract Cataract affecting the cortex of the lens. The opacities often begin as spokes or isolated dots or clusters forming the cuneiform or subcapsular types of cataract, but eventually the opacity spreads through the entire cortex.
cuneiform cataract Age-related cataract characterized by opacities distributed within the periphery of the cortex of the lens in a radial manner, like spokes on a wheel (Fig. C3). See subcapsular cataract.
cupuliform cataract See sub-capsular cataract.
diabetic cataract Cataract associated with diabetes. In old eyes this type is similar to that of a non-diabetic person but in young eyes it is typically of the snowflake type.
diffuse cataract See blue-dot cataract; Christmas tree cataract.
electric cataract An opacity caused by an electric shock.
cataract extraction, extracapsular (ECCE) Surgical procedure for the removal of a cataractous crystalline lens. The anterior capsule is excised, the lens nucleus is removed and the residual equatorial cortex is aspirated. The posterior capsule may be polished. An intraocular lens implant may then be inserted. See after-cataract; biometry of the eye; capsulectomy; intraocular lens; Elschnig's pearls; phacoemulsification; Soemmering's ring.
cataract extraction, intracapsular (ICCE) Surgical procedure for the removal of a cataractous crystalline lens. The entire lens, together with its capsule, is removed. This procedure is rarely performed nowadays. See ligament of Wieger.
fluid cataract Hypermature cataract in which the lens substance has degenerated into milky fluid.
glassblower's cataract See heat-ray cataract.
heat-ray cataract Cataract due to excessive exposure to heat and infrared radiation. Syn. glassblower's cataract; thermal cataract. See exfoliation of the lens; infrared.
hypermature cataract The last stage in the development of age-related cataract in which the lens substance has disintegrated. See incipient cataract; intumescent cortical cataract; mature cataract; phacolytic glaucoma.
incipient cataract The first stage in the development of age-related cataract characterized by streaks similar to the spokes of a wheel or with an increased density of the nucleus. See intumescent cortical cataract; mature cataract; crystalline lens; second sight.
intumescent cortical cataract A stage of development of a cataract in which the lens, especially the cortex, absorbs fluid and swells. It may lead to secondary angle-closure glaucoma. The cataract can progress to the hypermature stage in which case the fluid leaks out, resulting in shrinkage of the lens and wrinkling of the anterior capsule, leaving the harder nucleus free within the capsule. See morgagnian cataract.
lamellar cataract A congenital cataract affecting one layer of the crystalline lens only. Syn. zonular cataract.
mature cataract The middle stage in the development of age-related cataract characterized by a completely opaque lens and considerable loss of vision. See hypermature cataract; incipient cataract.
morgagnian cataract A hypermature age-related cataract in which the cortex has shrunk and liquefied and the nucleus floats within the lens capsule. Degraded lens proteins may leak into the aqueous humour and cause phacolytic glaucoma. Syn. cystic cataract; sedimentary cataract. See intumescent cortical cataract.
nuclear cataract An opacity affecting the lens nucleus. It can be either congenital or age-related in origin. It frequently leads to an increase in myopia (or decrease in hyperopia). In some cases it reaches such a brown colour that it is called brunescent cataract (or brown cataract). Syn. central cataract (Fig. C3).
polar cataract A congenital opacity found at either pole of the crystalline lens. Anterior polar cataract may be flat or project as a conical opacity (pyramidal cataract) into the anterior chamber (Fig. C3). Posterior types may be associated with persistent hyaloid remnant (Mittendorf's dot).
punctate cataract See blue-dot cataract.
pyramidal cataract See polar cataract.
senile cataract See age-related cataract.
secondary cataract 1. Syn. for complicated cataract. 2. Syn. for after-cataract.
snowflake cataract A cataract characterized by greyish or whitish flakelike opacities. It is usually found in young diabetics or severe cases of diabetes (Fig. C3).
soft cataract Cataract in which the lens nucleus is soft. See crystalline lens.
subcapsular cataract An age-related opacity located beneath the anterior or posterior capsule. It may spread from the periphery of the cortex like spokes on a wheel (cuneiform cataract). This is the most common type of cortical cataract. The opacities may also be confined to the posterior layers of the cortex with a granular or lace-like appearance (cupuliform cataract). Subcapsular cataracts are often the result of radiation exposure, age, toxic damage (e.g. from corticosteroids), or secondary to eye diseases (e.g. uveitis, retinitis pigmentosa). (Fig. C3).
sunflower cataract See chalcosis lentis.
cataract surgery See capsulectomy; capsulorhexis; capsulotomy; extracapsular cataract extraction; intracapsular cataract extraction; phacoemulsification.
sutural cataract A congenital cataract in which the opacities are found along the anterior and/or posterior lens sutures. The opacities may appear Y-shaped or flower-shaped. The condition is often associated with Fabry's disease.
thermal cataract See heat-ray cataract.
traumatic cataract Cataract following injury to the lens, its capsule, or to the eyeball itself. It is commonly unilateral. Penetrating trauma of the lens causes rapid opacification of the cortex or even most of the lens contents. Concussion of the lens may result in capsular, subcapsular or cortical opacities. See Vossius' ring.
zonular cataract See lamellar cataract.

cat·a·ract
(kat'ăr-akt)Patient discussion about cataract
Q. What Is a Cataract? My father has cataract in his eye, which interferes a lot with his vision. What is cataract?
Q. What vitamin through diet shall I take to prevent cataract and how can I help my dad? My father recently had a cataract surgery. This was his second cataract surgery. After this surgery I got scared as what’s going wrong with my dad and he had the cataract the second time. As per the doctor, my dad must be short in vitamins in his diet. He has been given some vitamin tablets. I know that cataract is genetic. I guess I may also have cataract in my old age. What vitamin through diet shall I take to prevent cataract and how can I help my dad?
http://www.youtube.com/watch?v=ezMQeIugWzY&eurl=http://www.imedix.com/health_community/vezMQeIugWzY_dissolve_cataracts_without_need_invasive_surgery_1?q=cataract&feature=player_embedded
Q. I had cataract surgery with iol implant, and ever since I have awful light sensitivity. Any ideas? I can't go into a "super store" without my sunglasses. My eyes ache at the end of the day. My doctor says "I don't know!"
cataract
[kat´ah-rakt]Blurred and dimmed vision are often the first symptoms. The patient may find that a brighter reading light is needed, or objects must be held closer to the eyes for better vision. Continued clouding of the lens may cause double vision; eventually there may be a need for frequent changes of eyeglasses. These symptoms do not necessarily indicate cataract, but if any of them are present, an ophthalmologist should be consulted immediately.
The lens of the eye serves only to focus light rays upon the retina. After cataract extraction the loss of the natural lens is compensated for by either special eyeglasses or contact lenses. Implantation of a permanent artificial lens, either during cataract surgery or later, is an alternative to use of cataract spectacles and a removable contact lens.
cat·a·ract
(kat'ă-rakt), Avoid the redundant phrase ocular cataract.Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp