Medical term:
cholecystectomies
Cholecystectomy
Definition
Purpose
Precautions
Description
Preparation
Aftercare
Key terms
Risks
Resources
Other
cholecystectomy
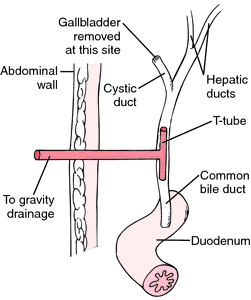
[ko″le-sis-tek´to-me]When the patient returns from surgery a careful check is made for drainage tubes inserted during the operation. Sometimes the drains are devised so that bile and serous fluid from the operative site drain directly onto the surgical dressings. Other drains or tubes such as a T-tube or Y-tube are attached to a drainage bag so that the amount of bile removed can be measured periodically. In either case, dressings over the wound are checked frequently for signs of bleeding or other abnormalities in the character and amount of drainage. When bile leakage is copious, as it sometimes is, the dressings will need to be reinforced and the outer layers changed as often as necessary to keep the patient dry and comfortable and to avoid irritation of the skin around the incision.
The nursing care plan of a patient with either a T-tube or a Y-tube should take into account three major potential problems: infection, obstruction, and dislodgment of the tube. Monitoring for infection includes watching for elevation of body temperature above 100° F and inspection of the tube insertion site for redness, swelling, warmth, and purulent drainage. The patient also is watched for jaundice and complaints of pain in the right upper quadrant, drainage around the tube when it is clamped, nausea, vomiting, and very dark urine and clay-colored stools, all of which indicate obstruction of the common bile duct. The amount of drainage from the tube is measured and recorded at least once every eight hours. A marked decrease in amount could mean that the tube has become dislodged.
Biliary tract disease continues to occur in approximately 5 to 8 per cent of all postcholecystectomy patients. The symptoms can appear within weeks after surgery or may occur years later and are the result of residual stones not removed at the time of surgery, newly formed gallstones, or stricture of the common bile duct. Infections and malignancies also can produce the symptoms of postcholecystectomy syndrome (PCS). Because of hormonal influences, women in the 40- to 49-year-old age group account for almost 80 per cent of patients with PCS. Treatment of the condition varies, but might entail more extensive surgery to provide a means by which bile can drain into the intestines.
cho·le·cys·tec·to·my
(kō'lē-sis-tek'tō-mē),cholecystectomy
(kō′lĭ-sĭ-stĕk′tə-mē)cholecystectomy
Surgery The surgical removal of the gallbladder Indications Gallstones, cholecystitis, cancer. See Bile, Cholecystitis, Gallstones, Laparoscopic cholecystectomy.cho·le·cys·tec·to·my
(kō'lĕ-sis-tek'tŏ-mē)cholecystectomy
(kō″lĕ-sis″tek′tŏ-mē) [ cholecyst- + -ectomy]
Acute, chronic, or acalculous cholecystitis (biliary inflammation that is not caused by gallstones), repeated episodes of biliary colic, biliary dyskinesia, gallstone pancreatitis, and occasionally cholangitis are indications for the procedure. The gallbladder does not usually need to be removed for asymptomatic gallstone disease.
Patient care
Preoperative: The patient is informed about the procedure, including the need for drains, catheter, nasogastric tubes, etc., and taught about incentive spirometry, leg exercises, incision splinting, analgesia use, and other postoperative concerns.
Postoperative: General patient care concerns apply. Vital signs are monitored and dressings are inspected. The patient is assessed for pain and for gastrointestinal and urinary function; analgesics and antiemetics are provided as needed. Fluid and electrolyte balance is monitored, and prescribed fluid replacement therapy is administered until the patient is permitted oral intake. The patient is encouraged to breathe deeply and to perform incentive spirometry to prevent atelectasis and impaired gas exchange. The patient is assisted with early ambulation and with splinting the abdomen when moving about or coughing. Peripheral circulation is evaluated, and venous return is promoted with leg exercises and elastic stockings or pneumatic hose as prescribed.
If a laparoscopic approach is used, the patient will typically be discharged the day of or the day after surgery. Clear liquids are offered after recovery from general anesthesia, and the patient resumes a normal diet within a few days. If an open incision is used, the patient is placed in a position of comfort; a nasogastric (NG) tube is frequently required to prevent abdominal distention and ileus, and is attached to low intermittent suction; and the volume and characteristics of drainage from the NG tube and any abdominal drains or T-tube are documented. Skin care and appropriate dressings are provided around any drain site.
When peristalsis returns, the NG tube is removed as directed. Oral intake, beginning with clear liquids, is initiated. The T-tube may be clamped before and after each meal to allow additional bile to enter the intestine. Signs and symptoms of postcholecystectomy syndrome (fever, abdominal pain, and jaundice) and other complications involving obstructed bile drainage are reported; urine and stool samples are collected for analysis of bile content should any such complications occur.
Discharge teaching for the patient and family includes wound care and T-tube care if appropriate (the T-tube may remain in place up to 2 weeks); the need to report any signs of biliary obstruction (fever, jaundice, pruritus, pain, dark urine, and clay-colored stools); the importance of daily exercise such as walking; avoidance of heavy lifting or straining for the prescribed period; and any restrictions on motor vehicle operation. Although diet is not restricted, the patient may be more comfortable avoiding excessive intake of fats and gas-forming foods for 4 to 6 weeks. Arrangements for home health follow-up or care may be necessary. The patient should return to the surgeon for a post-operative evaluation visit as scheduled. If gallstones were present, the patient is taught to reduce the risk of recurrence by maintaining normal body weight, exercising regularly, and eating three well-balanced meals daily, including fiber and calcium and avoiding alcohol and foods high in saturated fat. Weight loss, if needed, should be carried out gradually, and crash dieting discouraged.
extended cholecystectomy
laparoscopic laser cholecystectomy
Patient care
The nurse or surgeon explains to the patient that this type of surgery will not be used if the patient is pregnant or has had extensive abdominal surgery (because of concern for adhesions), severe acute cholecystitis, a palpable gallbladder, evidence of a stone in the common bile duct, or a bleeding problem. The patient is also told that the surgeon, using the endoscopic technique, will be able to remove the gallbladder without unsightly scarring, leaving only four (or less) small punctures, which reduces the risk for wound complications (infection, hematoma, separation). Risks for other complications (pneumonia, thrombophlebitis, urinary retention, and paralytic ileus) are also decreased because the procedure enables early mobility and may avoid use of parenteral analgesia. Patients will experience less pain and immobility, require less narcotic analgesia, be discharged on the same or on the next day, and be able to return to their usual activities (including work) within 7 days. Preoperative preparation, which usually is similar to that for any other abdominal surgery, is explained.
Postoperatively, the patient is stabilized during a brief stay in postanesthesia and then is transported to a surgical observation unit. The patient is offered clear liquids (carbonated beverages are avoided because they may cause distension and abdominal pressure). If the patient tolerates liquids, the IV is removed, and the patient is offered a regular diet. Analgesics are administered orally as prescribed as soon as the patient can take liquids. A parenteral narcotic (which may cause drowsiness, reduced intestinal motility, and/or vomiting) is given only if the patient continues to feel pain after taking an analgesic. Once the patient is comfortable, he is helped to walk because early ambulation speeds recovery. The patient is usually fully awake and walking within 3 or 4 hr of arrival on the unit. If he experiences shoulder pain, a heating pad may be applied. The surgeon, however, usually removes the carbon dioxide at the end of the procedure to prevent this problem. The nurse evaluates the patient's readiness for discharge, which usually can occur if the patient is afebrile, walking, eating, and voiding, and has stable vital signs with no evidence of bleeding or bile leakage. To assess for the latter risks, the patient is observed for severe pain and tenderness in the right upper quadrant, an increase in abdominal girth, leakage of bile-colored drainage from the puncture site, a fall in blood pressure, and increased heart rate
The patient is instructed to keep the adhesive bandages covering the puncture site clean and dry. He may remove them the next day and bathe or shower as usual. The patient most likely will require little analgesia, but a prescription is given for use as needed. He is reminded to pace activity according to energy level. While no special diet is required, the patient may wish to avoid excessive fat intake and gas-forming foods for 4 to 6 weeks. He should return to the surgeon for follow-up evaluation as directed and report any vomiting, abdominal distention, signs of infection, and new or worsening pain.
cholecystectomy
Surgical removal of the gall bladder.Patient discussion about cholecystectomy
Q. What is a cholecystectomy and how is it done? My Doctor diagnosed me with gallstones and said I have to have a cholecystectomy surgery. What is this and how is it done?
You will probably have a laparoscopic cholecystectomy, which means a surgeon will make a small slit in your abdomen, then insert a tubelike instrument which has a camera and surgical instruments attached. This is used to take out the gallbladder with the stones inside it.
This procedure causes less pain than open surgery, is less likely to cause complications, and has a faster recovery time. This surgery is performed in an operating room and you will be under general anesthesia. It usually takes 20 minutes to one hour.
Q. how people deal with after gallbladder removal
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp