Medical term:
erythrocyte
erythrocyte
[ĕ-rith´ro-sīt]The functions of erythrocytes include transportation of oxygen and carbon dioxide. They owe their oxygen-carrying ability to hemoglobin, a combination of an iron-containing prosthetic group (heme) with a protein (globin). Hemoglobin attracts and forms a loose connection with free oxygen, and its presence enables blood to absorb some 60 times the amount of oxygen that the plasma by itself absorbs. Oxyhemoglobin is red, which gives oxygenated blood its red color. Erythrocytes are stored in the spleen, which acts as a reservoir for the blood system and discharges the cells into the blood as required. The spleen may discharge extra erythrocytes into the blood during emergencies such as hemorrhage or shock.
Erythrocytes also are important in the maintenance of a normal acid-base balance, and, since they help determine the viscosity of the blood, they also influence its specific gravity. Their average life span is 120 days. They are subjected to much wear and tear in circulation and eventually are removed by cells of the reticuloendothelial system, particularly in the liver, bone marrow, and spleen. In spite of this constant destruction and production of erythrocytes, the body maintains a fairly constant number, between 4 and 5 million per mm3 of blood in women and 5 to 6 million per mm3 in men. A decreased number constitutes one form of anemia.
Erythrocytes are destroyed whenever they are exposed to solutions that are not isotonic to blood plasma. If they are placed in a solution that is more dilute than plasma (distilled water for example) the cells will swell until osmotic pressure bursts the cell membrane. If they are placed in a solution more concentrated than plasma, the cells will lose water and shrivel or crenate. It is for this reason that solutions to be given intravenously must be isotonic to plasma.
Aged red cells are ingested by macrophages in the spleen and liver. The iron is transported by the plasma protein transferrin to the bone marrow, where it is incorporated into new red cells. The heme group is converted to bilirubin, a bile pigment secreted by the liver. About 180 million red blood cells are destroyed every minute. Since the number of cells in the blood remains more or less constant, this means that about 180 million red blood cells are manufactured every minute.
Determination of the red blood cell volume is usually done as a preliminary step in determination of the total blood volume. A radioactive substance, usually chromium, is used to “tag” cells of a sample of blood drawn from the patient. The sample is then reintroduced into the circulating blood and subsequent samples are taken to be evaluated for degree of radioactivity. The degree of dilution is used to calculate total blood volume.
The erythrocyte sedimentation rate is often inconclusive and is not considered specific for any particular disorder. It is most often used as a gauge for determining the progress of an inflammatory disease such as rheumatic fever, rheumatoid arthritis, or a respiratory infection. The information provided by this test must be used in conjunction with results from other tests and clinical evaluations.
e·ryth·ro·cyte
(ĕ-rith'rō-sīt),erythrocyte
(ĭ-rĭth′rə-sīt′)erythrocyte
A mature, non-nucleated cell averaging 7–8 µm in diameter, which is round or ovoid on peripheral smear, contains haemoglobin and has a zone of central pallor due to the cell’s biconcavity. Erythrocytes are normally confined to blood vessels (aorta, arteries, arterioles, capillaries, venules, veins, inferior vena cava and superior vena cava), the heart and pulmonary vasculature. Haemoglobin, the main erythrocyte protein, is tasked with transporting O2 to tissues and CO2 away from tissues. Erythrocytes have an average lifespan of 120 days.erythrocyte
RBC, red blood cell, discocyte Hematology A mature, nonnucleated cell averaging 7–8 µm in diameter, which is round or ovoid on peripheral smear, contains Hb and has a zone of central pallor due to the cell's biconcavity. See Fetal erythrocyte.e·ryth·ro·cyte
(ĕ-rith'rŏ-sīt)Synonym(s): hemacyte, red blood cell, red cell, red corpuscle.
erythrocyte
(e-rith'ro-sit?) [ erythro- + -cyte]
Number
In a normal person, the number of erythrocytes averages about 5,000,000/µL (5,500,000 for men and 4,500,000 for women). The total number in an average-sized person is about 35 trillion. The number per µL varies with age (higher in infants), time of day (lower during sleep), activity and environmental temperature (increasing with both), and altitude. People living at altitudes of 10,000 ft (3048 m) or more may have an erythrocyte count of 8,000,000/µL or more.
If a person has a normal blood volume of 5 L (70 mL/ kg of body weight) and 5,000,000 erythrocytes per µL of blood, and the erythrocytes live 120 days, the red bone marrow must produce 2,400,000 erythrocytes per second to maintain this erythrocyte count.
Physiology
The primary function of erythrocytes is to carry oxygen. The hemoglobin also contributes to the acid-base balance of the blood by acting as a buffer for the transport of carbon dioxide in the plasma as bicarbonate ions.
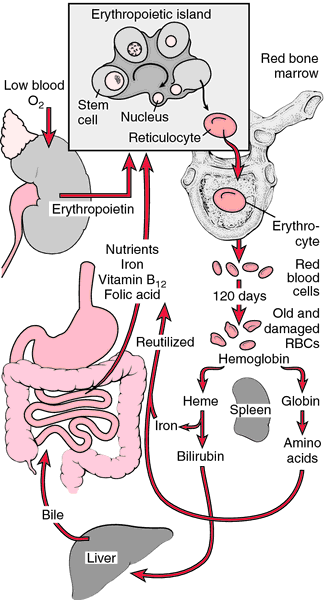
Development
Erythrocyte formation (erythropoiesis) in adults takes place in the bone marrow, principally in the vertebrae, ribs, sternum, hip bone, diploë of cranial bones, and proximal ends of the humerus and femur. erythrocytes arise from large nucleated stem cells (promegaloblasts), which give rise to pronormoblasts, in which hemoglobin appears. These become normoblasts, which extrude their nuclei. erythrocytes at this stage possess a fine reticular network and are known as reticulocytes. This reticular structure is usually lost before the cells enter circulation as mature erythrocytes. The proper formation of erythrocytes depends primarily on nutrition, with protein, iron, and copper essential for the formation of hemoglobin, and vitamin B12 and folic acid necessary for DNA synthesis in stem cells of the red bone marrow.
As erythrocytes age and become fragile, they are removed from circulation by macrophages in the liver, spleen, and red bone marrow. The protein and iron of hemoglobin are reused; iron may be stored in the liver until needed for the production of new erythrocytes in the bone marrow. The heme portion of the hemoglobin is converted to bilirubin, which is excreted in bile as one of the bile pigments.
Varieties
On microscopic examination, erythrocytes may reveal variations in the following respects: size (anisocytosis), shape (poikilocytosis), staining reaction (achromia, hypochromia, hyperchromia, polychromatophilia), structure (possession of bodies such as Cabot's rings, Howell-Jolly bodies, Heinz bodies; parasites such as malaria; a reticular network; or nuclei), and number (anemia, polycythemia).
achromatic erythrocyte
basophilic erythrocyte
crenated erythrocyte
immature erythrocyte
orthochromatic erythrocyte
polychromatic erythrocyte
erythrocyte
A red blood cell. ‘Erythro’ means ‘red’, and ‘cyte’ means ‘cell’. Erythrocytes are flattened discs, slightly hollowed on each side (biconcave) and about 7 thousandths of a millimetre in diameter. They contain HAEMOGLOBIN and their main function is to transport OXYGEN from the lungs to the tissues.
erythrocyte or red blood cell (RBC)
a vertebrate cell that contains HAEMOGLOBIN pigment for oxygen transport from lungs to tissues and carries small amounts of carbon dioxide as HCO3 - from tissues to lungs (see also CHLORIDE SHIFT). Unlike other vertebrate cells, mammalian RBCs are non-nucleated and have definite biconcave shape. Compare LEUCOCYTE.Erythrocyte
e·ryth·ro·cyte
(ĕ-rith'rŏ-sīt)Synonym(s): hemacyte, red blood cell, red cell, red corpuscle.
Patient discussion about erythrocyte
Q. what is a normal red blood cell count for breast cancer after operation
Latest Searches:
viscosity - viscosimetry - viscosimeter - viscose - viscometry - viscometer - Viscoheel - viscogel - viscoelasticity - viscoelastic - Viscoat - viscidity - viscid - visci - viscerum - viscerotropic - viscerotrophic - viscerotonia - viscerotomy - viscerotome -
- Service manuals - MBI Corp