Medical term:
intracranial
intracranial
[in″trah-kra´ne-al]within the cranium.
intracranial pressure (ICP) the pressure of the cerebrospinal fluid in the subarachnoid space, the space between the skull and the brain; the normal range is between 50 and 180 mm H2O (approximately 4 to 13 mm Hg). A reading above 200 mm H2O (about 15 mm Hg) is considered abnormally high; however, intracranial pressure, like arterial blood pressure, can fluctuate markedly and quickly during certain activities. For example, a transient elevation of pressure occurs during valsalva's maneuver. Straining at stool, isometric exercises, and similar activities can momentarily raise the intracranial pressure to as high as 1360 mm H2O. While signs of sustained increased intracranial pressure can be significant in the assessment of a patient with a neurologic disorder, momentary increases in intracranial pressure are not in themselves necessarily detrimental.
The level of intracranial pressure can be inferred by determining the pressure of lumbar spinal fluid during a spinal tap, but this is not the most accurate method and it can be dangerous. Removal of even a small amount of spinal fluid from a patient with a significantly high intracranial pressure can alter the pressure difference between the spinal column and the cranial cavity and cause herniation of the midbrain downward into the foramen magnum. A more accurate and continuous measurement of intracranial pressure can be obtained by monitoring pressure within the cerebral ventricles (cerebral ventricular pressure).
The level of intracranial pressure can be inferred by determining the pressure of lumbar spinal fluid during a spinal tap, but this is not the most accurate method and it can be dangerous. Removal of even a small amount of spinal fluid from a patient with a significantly high intracranial pressure can alter the pressure difference between the spinal column and the cranial cavity and cause herniation of the midbrain downward into the foramen magnum. A more accurate and continuous measurement of intracranial pressure can be obtained by monitoring pressure within the cerebral ventricles (cerebral ventricular pressure).
Causes of Increase in Pressure. The skull is a rigid container that holds the brain, blood vessels, and cerebrospinal fluid. There is room for some expansion within the skull, but not much, and any condition that causes an increase in volume in one or more of the structures within the cranium will cause an increase in pressure within the contained area. A tumor or swelling of brain tissue can increase the volume, as can extravascular leakage of blood and the formation of clots, dilatation of the cerebral vessels, and excess production, impeded outflow, or insufficient absorption of cerebrospinal fluid, as in hydrocephalus.
Increased fluid volume creates pressure against the structures inside the cranium, disrupting the blood and oxygen supply, and resulting in cellular hypoxia. As the pressure increases, the brain mass shifts or is distorted, causing compression of the neurons and nerve tracts or of the cerebral arteries. The effect of increased volume can be generalized, as in brain edema from lead poisoning, or focal. Cellular hypoxia resulting from direct pressure on the brain cells, distortion of the brain mass, or occlusion of cerebral blood vessels accounts for the signs and symptoms of increased intracranial pressure. A sustained increase in the pressure causes persistent hypoxia, irreversible damage to the brain cells, and eventually death.
Increased fluid volume creates pressure against the structures inside the cranium, disrupting the blood and oxygen supply, and resulting in cellular hypoxia. As the pressure increases, the brain mass shifts or is distorted, causing compression of the neurons and nerve tracts or of the cerebral arteries. The effect of increased volume can be generalized, as in brain edema from lead poisoning, or focal. Cellular hypoxia resulting from direct pressure on the brain cells, distortion of the brain mass, or occlusion of cerebral blood vessels accounts for the signs and symptoms of increased intracranial pressure. A sustained increase in the pressure causes persistent hypoxia, irreversible damage to the brain cells, and eventually death.
Signs and Symptoms. The four classic groups of intracranial signs of increased intracranial pressure are (1) altered levels of consciousness; (2) changes in sensory and motor function; (3) changes in pupil size, equality, and reaction to light, and extraocular movements; and (4) changes in vital signs and patterns of respiration. However, only a few of these signs occur early in the process and then usually only at peak pressures.
Altered levels of consciousness occur as a result of compression of the ascending reticular activating system pathways and the resulting hypoxia of the cells of these tissues as well as the cells of the cortex. As compression increases the patient becomes more difficult to arouse. Assessment of the patient is based on the extent to which he is oriented and able to respond to stimuli. (See also levels of consciousness.)
Motor and sensory dysfunction are the result of pressure on the cortex and the upper motor and sensory pyramidal pathways. The motor fibers descend through the brain stem where most of them cross over (decussate) in the medulla oblongata and then extend into the spinal cord. Sensory fibers ascend from the spinal cord to the brain stem and from there to the sensory areas in the parietal lobe of the brain. These fibers also decussate in either the spinal cord or the medulla. Assessment of the patient for motor and sensory dysfunction would include an evaluation of movement and strength of the extremities and a comparison of right side to left; perception of touch, pressure, and deep pain; and the presence or absence of the babinski reflex.
Changes in pupil size, equality, and reaction to light, and extraocular movements are indicative of compression of the third, fourth, and sixth cranial nerves. Assessment of these changes should be as accurate and objective as possible. Unilateral and bilateral evaluations are important and usually are recorded by a drawing of the actual size of each pupil or by precise measurements using a small metric ruler.
Vital sign changes come very late in the process of cellular hypoxia and indicate that pressure is being exerted on the lower brain stem and medulla. If not relieved, these changes quickly accelerate and death ensues. Compression of the brain stem causes a rise in the systolic blood pressure and a widening of the pulse pressure followed by a sharp drop in blood pressure. The pulse rate slows and then rises sharply owing to blocking of the parasympathetic impulses. As pressure on the respiratory center builds up there are changes in the rate, rhythm, and ratio of inspiration to expiration, and periods of apnea.
Earlier in the process, more subtle changes in the neurologic status of the patient can be detected by an experienced practitioner and are extremely important for prompt intervention and correction of the problem before irreversible damage is done. Signs and symptoms frequently noted early in the process and at peak pressure include increased restlessness, mental dullness, disorganized and unfocused behavior, such as plucking at the bedclothes, and increasingly severe headache. Another significant event is a transient worsening of the neurologic status as indicated by changes in the four classic signs and symptoms. These transient changes reflect a situation in which a critical volume of intracranial contents has been reached; small increases beyond that point are likely to lead to rapid and sustained increases in pressure. This situation demands immediate intervention for relief of compression of vital neuronal structures.
Altered levels of consciousness occur as a result of compression of the ascending reticular activating system pathways and the resulting hypoxia of the cells of these tissues as well as the cells of the cortex. As compression increases the patient becomes more difficult to arouse. Assessment of the patient is based on the extent to which he is oriented and able to respond to stimuli. (See also levels of consciousness.)
Motor and sensory dysfunction are the result of pressure on the cortex and the upper motor and sensory pyramidal pathways. The motor fibers descend through the brain stem where most of them cross over (decussate) in the medulla oblongata and then extend into the spinal cord. Sensory fibers ascend from the spinal cord to the brain stem and from there to the sensory areas in the parietal lobe of the brain. These fibers also decussate in either the spinal cord or the medulla. Assessment of the patient for motor and sensory dysfunction would include an evaluation of movement and strength of the extremities and a comparison of right side to left; perception of touch, pressure, and deep pain; and the presence or absence of the babinski reflex.
Changes in pupil size, equality, and reaction to light, and extraocular movements are indicative of compression of the third, fourth, and sixth cranial nerves. Assessment of these changes should be as accurate and objective as possible. Unilateral and bilateral evaluations are important and usually are recorded by a drawing of the actual size of each pupil or by precise measurements using a small metric ruler.
Vital sign changes come very late in the process of cellular hypoxia and indicate that pressure is being exerted on the lower brain stem and medulla. If not relieved, these changes quickly accelerate and death ensues. Compression of the brain stem causes a rise in the systolic blood pressure and a widening of the pulse pressure followed by a sharp drop in blood pressure. The pulse rate slows and then rises sharply owing to blocking of the parasympathetic impulses. As pressure on the respiratory center builds up there are changes in the rate, rhythm, and ratio of inspiration to expiration, and periods of apnea.
Earlier in the process, more subtle changes in the neurologic status of the patient can be detected by an experienced practitioner and are extremely important for prompt intervention and correction of the problem before irreversible damage is done. Signs and symptoms frequently noted early in the process and at peak pressure include increased restlessness, mental dullness, disorganized and unfocused behavior, such as plucking at the bedclothes, and increasingly severe headache. Another significant event is a transient worsening of the neurologic status as indicated by changes in the four classic signs and symptoms. These transient changes reflect a situation in which a critical volume of intracranial contents has been reached; small increases beyond that point are likely to lead to rapid and sustained increases in pressure. This situation demands immediate intervention for relief of compression of vital neuronal structures.
Patient Care. In addition to a thorough understanding of the pathophysiologic changes brought on by increased intracranial pressure and the signs and symptoms they produce, the nurse and other health professionals should be aware of factors that can precipitate increases in intracranial pressure. It is known, for example, that hypercapnia, profound hypoxia, and certain anesthetics can cause vasodilation of cerebral vessels and an increase in intracranial pressure. Patients who are known to be at risk for increases in pressure should not be given vasodilating drugs whenever such therapy can be avoided. The blood gases and chest sounds of these patients should be monitored periodically to determine whether there is adequate ventilation and oxygenation. Maintenance of a patent airway and adequate oxygenation by means of oxygen therapy, if necessary, are essential to the prevention of an escalating intracranial pressure.
Other protective measures for patients at risk for sudden increases in intracranial pressure include careful positioning to avoid flexion of the neck, extreme flexion of the hip, or the prone position. Elevating the head 15 to 30 degrees decreases baseline pressure. The patient also should avoid the Valsalva maneuver when moving about in bed and when defecating. Isometric exercises to avoid the hazards of immobility are contraindicated but passive range-of-motion exercises are not.
Other protective measures for patients at risk for sudden increases in intracranial pressure include careful positioning to avoid flexion of the neck, extreme flexion of the hip, or the prone position. Elevating the head 15 to 30 degrees decreases baseline pressure. The patient also should avoid the Valsalva maneuver when moving about in bed and when defecating. Isometric exercises to avoid the hazards of immobility are contraindicated but passive range-of-motion exercises are not.
intracranial pressure monitoring
1. ICP monitoring; continuous monitoring of intracranial pressure. The three basic techniques used are intraventricular, subarachnoid (subdural), and epidural, with the intraventricular technique being the most common.
2. in the nursing interventions classification, a nursing intervention defined as the measurement and interpretation of patient data to regulate intracranial pressure.
In ICP monitoring, ventricular-fluid pressures are recorded from a zero baseline; the normal range is 0 to 15 mm Hg. Pressures usually are expressed in mm Hg rather than mm H2O in order to facilitate comparison with mean systemic arterial pressures. The difference between mean ventricular pressure and mean arterial pressure indicates the pressure at which the brain is being perfused with blood.
ICP monitoring gives a far more accurate picture of forces at work within the closed cranial cavity than does clinical observation of the patient for signs of increased intracranial pressure. Most authorities agree that dangerously high levels of intracranial pressure exist well before clinical symptoms become evident. Invasive monitoring of pressure also provides access for cerebrospinal fluid drainage to relieve pressure, for procurement of samples of cerebrospinal fluid for laboratory evaluations, and for observation of volume--pressure responses to therapeutic intervention.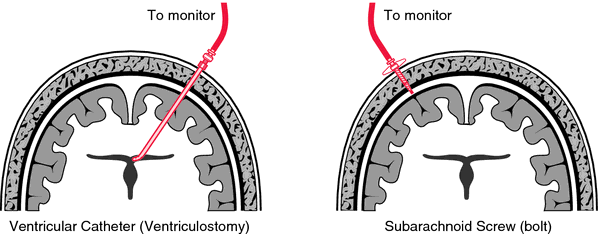
In ICP monitoring, ventricular-fluid pressures are recorded from a zero baseline; the normal range is 0 to 15 mm Hg. Pressures usually are expressed in mm Hg rather than mm H2O in order to facilitate comparison with mean systemic arterial pressures. The difference between mean ventricular pressure and mean arterial pressure indicates the pressure at which the brain is being perfused with blood.
ICP monitoring gives a far more accurate picture of forces at work within the closed cranial cavity than does clinical observation of the patient for signs of increased intracranial pressure. Most authorities agree that dangerously high levels of intracranial pressure exist well before clinical symptoms become evident. Invasive monitoring of pressure also provides access for cerebrospinal fluid drainage to relieve pressure, for procurement of samples of cerebrospinal fluid for laboratory evaluations, and for observation of volume--pressure responses to therapeutic intervention.
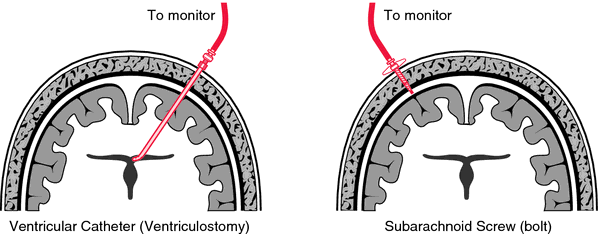
Intracranial pressure monitoring. From Polaski and Tatro, 1996.
intracranial pressure screw a device for measuring the degree of pressure being exerted within the subarachnoid space. Monitoring can be done on a continuous or an intermittent basis. The screw is inserted through a burr hole in the frontal area of the skull just behind the hairline and a capped 3-way stop cock is attached to the pressure screw. High-pressure tubing joined to the screw leads to a manometer on which pressure changes can be directly visualized, or to equipment which displays the information on an oscilloscope or graph. Readings on changes in intracranial pressure can thus be obtained by watching the manometer or by monitoring the oscilloscope or graphic display. When the manometer is used, point zero is established after positioning the patient with the head of the bed elevated 30 degrees.
Through the use of the intracranial pressure screw, elevations in intracranial pressure can be detected before changes in the vital signs and other symptoms of increased pressure become apparent. In this way measures can be taken to reduce the pressure before irreversible damage is done to the brain tissue.
The major risks of the intracranial pressure screw are infection and leakage of cerebrospinal fluid, either of which necessitates removal of the screw.
Through the use of the intracranial pressure screw, elevations in intracranial pressure can be detected before changes in the vital signs and other symptoms of increased pressure become apparent. In this way measures can be taken to reduce the pressure before irreversible damage is done to the brain tissue.
The major risks of the intracranial pressure screw are infection and leakage of cerebrospinal fluid, either of which necessitates removal of the screw.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
in·tra·cra·ni·al
(in'tră-krā'nē-ăl),Within the cranium, usually meaning within the cranial cavity.
Farlex Partner Medical Dictionary © Farlex 2012
intracranial
(ĭn′trə-krā′nē-əl)adj.
Occurring or situated within the cranium.
in′tra·cra′ni·al·ly adv.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
intracranial
adjective Within the skull.Segen's Medical Dictionary. © 2012 Farlex, Inc. All rights reserved.
intracranial
Within the skull.Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005
Intracranial
Located within or on the surface of the brain.
Mentioned in: Brain Tumor
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
in·tra·cra·ni·al
(in'tră-krā'nē-ăl)Within the cranium, usually meaning within the cranial cavity.
Medical Dictionary for the Dental Professions © Farlex 2012
Word not found in the Dictionary and Encyclopedia. Did you mean:
- intracranially
- intracranial
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp