Medical term:
osteoarthritis
Osteoarthritis
Definition
Description
Causes and symptoms
Primary osteoarthritis
Secondary osteoarthritis
- trauma, including sports injuries
- repetitive stress injuries associated with certain occupations (like the performing arts, construction or assembly line work, computer keyboard operation, etc.)
- repeated episodes of gout or septic arthritis
- poor posture or bone alignment caused by developmental abnormalities
- metabolic disorders
Diagnosis
History and physical examination
Diagnostic imaging
Treatment
Patient education and psychotherapy
Medications
Physical therapy

Surgery
Protective measures
New treatments
- Disease-modifying drugs. These compounds may be useful in assisting the body to form new cartilage or improve its repair of existing cartilage.
- Hyaluronic acid. Injections of this substance may help to lubricate and protect cartilage, thereby promoting flexibility and reduced pain. These agents include hyaluronan (Hyalgan) and hylan G-F20 (Synvisc).
- Cartilage transplantation. This technique is presently used in Sweden.
Alternative treatment
Diet
Nutritional supplements
Naturopathy
Traditional chinese medicine (tcm)
Other alternatives
- transcutaneous electrical nerve stimulation (TENS)
- magnet therapy
- therapeutic touch
- acupuncture
- yoga
Prognosis
Key terms
Resources
Periodicals
osteoarthritis
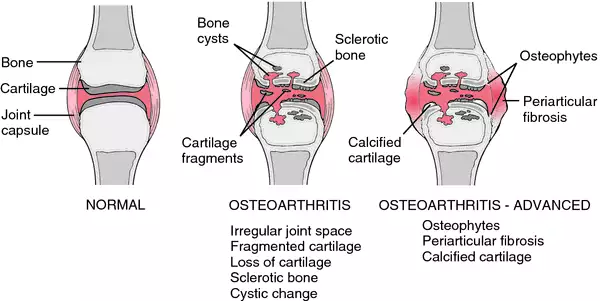
[os″te-o-ahr-thri´tis]Symptoms vary from mild to severe, depending on the amount of degeneration that has taken place. Osteoarthritis is caused by disintegration of the cartilage that covers the ends of the bones. As the cartilage wears away, the roughened surface of the bone is exposed, and pain and stiffness result. In severe cases the center of the bone wears away and a bony ridge is left around the edges. This ridge may restrict movement of the joint. Osteoarthritis is less crippling than rheumatoid arthritis, in which two bone surfaces may fuse, completely immobilizing the joint.
Treatment is aimed at preventing crippling deformities, relieving pain, and maintaining motion of the joint; see also treatment of arthritis.
os·te·o·ar·thri·tis
(os'tē-ō-ar-thrī'tis), [MIM*165720] This word is a misnomer in that the dominant pathologic process is degeneration rather than inflammation.osteoarthritis
(ŏs′tē-ō-är-thrī′tĭs)osteoarthritis
Degenerative arthritis, degenerative joint disease, hypertrophic osteoarthritis, noninflammatory arthritis, osteoarthrosis wear-and-tear arthritis Orthopedics The most common type of arthritis characterized by inflammation, degeneration and eventual loss of the cartilage of the joints of finger, hands, feet, spine, and large weight-bearing joints–eg, hips and knees, local pain, without systemic disease Etiology Unknown; aging, metabolic, genetic, chemical, mechanical factors may play a role. See Cervical osteoarthritis. Cf Rheumatoid arthritis.os·te·o·ar·thri·tis
(os'tē-ō-ahr-thrī'tis)Synonym(s): degenerative joint disease, hypertrophic arthritis, osteoarthrosis.
osteoarthritis
(os?te-o-ar-thri'tis ) [? + arthron, joint, + itis, inflammation],OA

Patient care
Treatment is supportive, using exercise balanced with rest and locally applied heat. Weight reduction, if needed, can ease joint pain and improve mobility; a body mass index below 24.9 is desirable. Aerobic exercise and flexibility routines can prevent joint stiffness related to lack of movement, and strong muscles provide better joint support. Swimming and aquatic exercises, which improve aerobic fitness without stressing joints, are encouraged. Meditation and other forms of relaxation may be beneficial as part of the patient's daily routine. Analgesics provide pain relief. Acetaminophen is the drug of choice, unless contraindicated. Nonsteroidal anti-inflammatory drugs (NSAIDs) are good alternatives for pain that is unresponsive to acetaminophen, although these agents increase the risk of gastrointestinal injury, bleeding, and renal failure. Other useful drugs include low doses of narcotic pain relievers, steroids, and intra-articular injections. Some patients, esp. those with osteoarthritis of the knee, benefit from joint bracing. If degeneration reaches the point where a joint is “bone on bone, ” joint replacement surgery usually is recommended, providing greatly improved mobility and function as well as pain relief.
osteoarthritis
A common form of persistent degenerative joint disease involving damage to the cartilaginous bearing surfaces and sometimes widening or remodelling of the ends of the bones involved in the joint. RHEUMATOID FACTOR is not present in the blood. Osteoarthritis is an age-related condition and affects especially those joints that have previously been damaged.os·te·o·ar·thri·tis
(os'tē-ō-ahr-thrī'tis) [MIM*165720]Synonym(s): arthrosis (2) .
Patient discussion about osteoarthritis
Q. What are the complications of osteoarthritis? I have been suffering from osteoarthritis for over a year now. What are the complications of this disease?
Q. What Are the Possible Treatments for Osteoarthritis? My sister is suffering from osteoarthritis. What are the possible treatments for this disease?
My Mother has had osteoarthritis for about 20years. She has tried numerous things to allieviate the pain she has had. About three months ago, she started taking a natural product for inflammation. She still has osteoarthritis, but the pain has reduced so much that she is now able to do so many things she hasn't been able to do in a long time. She can now put pegs on the clothes line, turn light switches on/off, open bottles. I really feel for yourself and other who have osteoarthritis. I never really understood how debilitating it can be. I hope you tell people that you are in pain. I never knew my mother couldn't do all these things.
Best of luck,
Kathryn
Q. Can knee pain at childhood be connected to osteoarthritis? My mother is suffering from osteoarthritis (OA). She is 72 years old and the OA is a major problem in her life. My son is 10 years old. He has a relapsing knee pain. His pain occurs mostly at day time but can wake him from sleep. The pain is in both legs. Is my son in a risk group for OA?
http://www.5min.com/Video/The-Fat-Burning-Formula-For-Women---week-6-13962180
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp