Medical term:
pepsic
peptic
[pep´tik]1. pertaining to pepsin.
2. pertaining to digestion by or other action of gastric juices.
peptic ulcer a loss of tissues lining the lower esophagus, stomach, or duodenum; an acute lesion that does not extend through the muscularis mucosae is simply called an erosion. Chronic ulcers involve the muscular coat, destroying the musculature and replacing it with permanent scar tissue at the site of healing.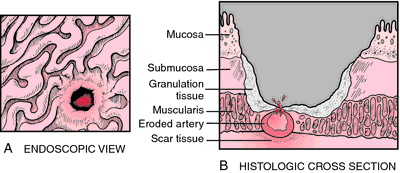
Cause. While it is known that gastric hydrochloric acid and pepsin are responsible for ulcer formation, it is not known why mucosal resistance to them should become impaired. Duodenal ulcers and some prepyloric gastric ulcers are associated with an increased amount or hyperacidity of the gastric juice. Gastric ulcers, on the other hand, are not associated with excessive acid levels. Theories about genetic and environmental causes of peptic ulcer abound. Both gastric and duodenal ulcers tend to occur in families. Relatives of persons with gastric ulcers have three times the expected number of gastric ulcers. The same is true of duodenal ulcers. There is evidence that the increased familial incidence of both gastric and duodenal ulcers is not just due to a shared environment. An infection with Helicobacter pylori may contribute to ulceration, particularly in persons with a history of chronic gastritis.
Psychosomatic factors are known to play some role in the development of peptic ulcers. Psychologic stress can and does alter gastric function. Prolonged psychologic or physiologic stress produces what is known as a stress ulcer, which differs pathologically and clinically from a chronic peptic ulcer in being more acute and more likely to produce hemorrhage; perforation occurs occasionally and pain is rare. Conditions often associated with stress ulcers include severe trauma, surgery, advanced malignancy, extensive burns (Curling's ulcer), and brain injury.
Drug-induced ulcers are most commonly caused by the ingestion of aspirin, with alcohol running a close second. Other drugs that are strongly suspected of being ulcerogenic include the glucocorticoids, indomethacin, and phenylbutazone.
Psychosomatic factors are known to play some role in the development of peptic ulcers. Psychologic stress can and does alter gastric function. Prolonged psychologic or physiologic stress produces what is known as a stress ulcer, which differs pathologically and clinically from a chronic peptic ulcer in being more acute and more likely to produce hemorrhage; perforation occurs occasionally and pain is rare. Conditions often associated with stress ulcers include severe trauma, surgery, advanced malignancy, extensive burns (Curling's ulcer), and brain injury.
Drug-induced ulcers are most commonly caused by the ingestion of aspirin, with alcohol running a close second. Other drugs that are strongly suspected of being ulcerogenic include the glucocorticoids, indomethacin, and phenylbutazone.
Symptoms. The cardinal symptom of peptic ulcer is epigastric pain that may be described as burning, gnawing, cramping, or aching, and usually comes in waves that last several minutes. The daily pattern of pain is related to the secretion of acid and the presence of food in the stomach to act as a buffer. This pain is diminished in the morning when secretion is low and after meals when food is present. The pain is most severe before meals and at bedtime. It often appears for three or four days or weeks and then subsides only to reappear weeks or months later. Other symptoms of uncomplicated peptic ulcer include nausea, loss of appetite, and sometimes weight loss.
Complications. The three major complications of ulcer are hemorrhage, perforation, and obstruction. Bleeding may be manifested by emesis of bright red blood or of coffee-ground vomitus, and by tarry feces. The bleeding may vary from massive hemorrhage to occult (hidden) bleeding that occurs over a period of time. Perforation frequently is a surgical emergency because of the possibility of a chemical peritonitis caused by spilling of the gastric and intestinal contents into the peritoneal cavity. Obstruction of the upper intestinal tract occurs as a result of scarring and loss of musculature at the pylorus. It is manifested by persistent vomiting that can quickly bring on alkalosis because of the loss of gastric acid in the vomitus. The obstruction is treated by surgical removal of the scar tissue.
Diagnosis. The most commonly used technique in the diagnosis of peptic ulcers is an upper gastrointestinal series with a barium test (barium swallow). Double contrast films are sometimes done to clearly define the mucosal pattern in the upper gastrointestinal tract. gastroscopy may be helpful in establishing the site of bleeding in a gastric ulcer, in differentiating between benign and malignant ulcerations based on biopsies, and between esophageal ulcer and diverticulum. Gastric analysis to determine level of acidity may be helpful in some cases but there is much individual variation in gastric acid secretions among patients with ulcer.
Treatment. The primary goals of medical treatment of peptic ulcers are: (1) relief of symptoms, (2) promotion of healing, (3) prevention of complications, and (4) prevention of recurrences. Because each patient responds differently to various modes of treatment, the medical regimen is planned according to individual needs and responses.
In general the medical management of ulcers hinges on antacids, drugs such as cimetidine that are antagonistic to histamine H2receptors, anticholinergic drugs, and sedatives; this is also accompanied by dietary modification and identifying and relieving sources of psychologic stress. Antacids such as magnesium hydroxide and aluminum hydroxide relieve the pain of ulcer by decreasing the levels of gastric hydrochloric acid and pepsin.
Cimetidine is an antagonist of histamine H2receptors and inhibits gastric acid secretion; it is easier to take than liquid antacids. It is an effective treatment for peptic ulcers but produces side effects in some patients, e.g., breast enlargement in men, mental confusion in elderly patients, and delayed hepatic metabolism of other drugs. sucralfate, which is not absorbed into the body, is an alternative drug that has fewer side effects and is also effective. Another drug, ranitidine, has action similar to that of cimetidine, but has greater potency, can be taken less frequently, and has fewer side effects.
If Helicobacter pylori is found in the ulcer, the patient is treated with antibiotics.
Most ulcers can be treated without surgery when patients cooperate fully; however, surgery may be necessary in certain cases, such as when there is scarring of the ulcer (producing obstruction), recurrent bleeding, extreme pain, and perforation. Gastric ulcers are more likely to require surgery than are duodenal ulcers. The operative procedure most frequently done for a gastric ulcer is subtotal gastrectomy, in which the ulcerous portion of the stomach is removed (see also surgery of the stomach). This procedure is often done in conjunction with vagotomy, division of the vagus nerve, which eliminates cerebral stimuli of the stomach muscle and glands, thereby reducing gastric motility and secretion.
In general the medical management of ulcers hinges on antacids, drugs such as cimetidine that are antagonistic to histamine H2receptors, anticholinergic drugs, and sedatives; this is also accompanied by dietary modification and identifying and relieving sources of psychologic stress. Antacids such as magnesium hydroxide and aluminum hydroxide relieve the pain of ulcer by decreasing the levels of gastric hydrochloric acid and pepsin.
Cimetidine is an antagonist of histamine H2receptors and inhibits gastric acid secretion; it is easier to take than liquid antacids. It is an effective treatment for peptic ulcers but produces side effects in some patients, e.g., breast enlargement in men, mental confusion in elderly patients, and delayed hepatic metabolism of other drugs. sucralfate, which is not absorbed into the body, is an alternative drug that has fewer side effects and is also effective. Another drug, ranitidine, has action similar to that of cimetidine, but has greater potency, can be taken less frequently, and has fewer side effects.
If Helicobacter pylori is found in the ulcer, the patient is treated with antibiotics.
Most ulcers can be treated without surgery when patients cooperate fully; however, surgery may be necessary in certain cases, such as when there is scarring of the ulcer (producing obstruction), recurrent bleeding, extreme pain, and perforation. Gastric ulcers are more likely to require surgery than are duodenal ulcers. The operative procedure most frequently done for a gastric ulcer is subtotal gastrectomy, in which the ulcerous portion of the stomach is removed (see also surgery of the stomach). This procedure is often done in conjunction with vagotomy, division of the vagus nerve, which eliminates cerebral stimuli of the stomach muscle and glands, thereby reducing gastric motility and secretion.
Patient Care. Assessment data pertinent to peptic ulcer patients include information about (1) family history of peptic ulcer, (2) the patient's eating habits and how eating affects symptoms, (3) whether the patient drinks or smokes and to what extent, (4) any history of psychological or physical stress such as severe trauma, burns, or other conditions that might produce a stress ulcer, and (5) any drugs the patient might be taking that are irritants to the gastrointestinal tract.
Dietary restrictions are usually limited to those foods, if any, that an individual identifies with the onset or worsening of symptoms. Exceptions are alcohol and caffeine, both of which are capable of inducing gastritis and promoting erosion of the gastric mucosa. It is generally agreed that what the patient with an ulcer eats is not as important as when it is eaten. Frequent and regular feedings throughout the day, rather than two or three large meals, are encouraged. Patients should not skip meals and should try to have some nonirritating food in the stomach at all times.
Patient education includes the following: (1) Regulate the types of foods eaten and the manner in which they are eaten. Meals should be unhurried, relaxed, and spaced at regular intervals. (2) Try to avoid situations of stress and anxiety and develop some effective skills for coping with stress. (3) Drink water at least once every hour when awake. This acts to dilute gastric juices, making them less corrosive. (4) Stop or at least cut down on smoking. (5) Keep alcohol intake to a minimum. (6) Report any side effects of antacids or other drugs to the health care provider. There are alternative drugs if the side effects of one are worrisome. (7) Take prescribed medications exactly as ordered and do not discontinue them without consulting the health care provider. (8) Avoid taking aspirin; develop the habit of reading labels of nonprescription drugs to ascertain whether they contain acetylsalicylic acid. Since some prescription drugs also contain aspirin, inform any health care provider treating a coexisting condition that aspirin cannot be tolerated.
Dietary restrictions are usually limited to those foods, if any, that an individual identifies with the onset or worsening of symptoms. Exceptions are alcohol and caffeine, both of which are capable of inducing gastritis and promoting erosion of the gastric mucosa. It is generally agreed that what the patient with an ulcer eats is not as important as when it is eaten. Frequent and regular feedings throughout the day, rather than two or three large meals, are encouraged. Patients should not skip meals and should try to have some nonirritating food in the stomach at all times.
Patient education includes the following: (1) Regulate the types of foods eaten and the manner in which they are eaten. Meals should be unhurried, relaxed, and spaced at regular intervals. (2) Try to avoid situations of stress and anxiety and develop some effective skills for coping with stress. (3) Drink water at least once every hour when awake. This acts to dilute gastric juices, making them less corrosive. (4) Stop or at least cut down on smoking. (5) Keep alcohol intake to a minimum. (6) Report any side effects of antacids or other drugs to the health care provider. There are alternative drugs if the side effects of one are worrisome. (7) Take prescribed medications exactly as ordered and do not discontinue them without consulting the health care provider. (8) Avoid taking aspirin; develop the habit of reading labels of nonprescription drugs to ascertain whether they contain acetylsalicylic acid. Since some prescription drugs also contain aspirin, inform any health care provider treating a coexisting condition that aspirin cannot be tolerated.
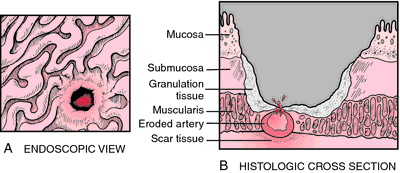
Peptic ulcer. A, Gross appearance of the ulcer as seen by endoscopy. B, Histologically, the bottom of the ulcer replacing the mucosa consists mostly of granulation tissue and admixed necrotic cell debris and inflammatory cells. Peptic ulcer may bleed from eroded mucosa blood vessels. The tissue underlying the ulcer shows fibrosis and scarring. From Damjanov, 2000.
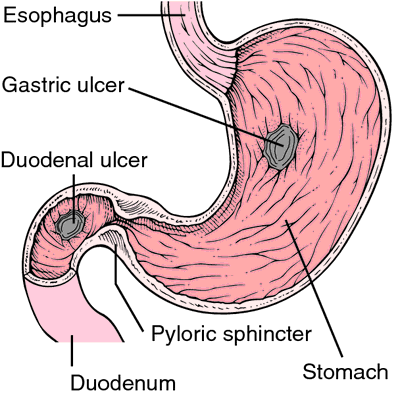
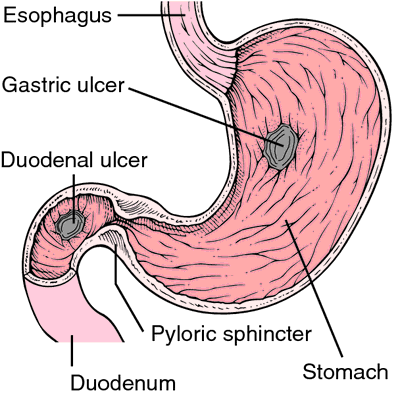
Most common sites for peptic ulcer disease. From Frazier et al., 2000.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
pep·tic
(pep'tik),Relating to the stomach, to gastric digestion, or to pepsin A.
Synonym(s): pepsic
[G. peptikos, fr. peptō, to digest]
Farlex Partner Medical Dictionary © Farlex 2012
peptic
(pĕp′tĭk)adj.
1.
a. Of, relating to, or assisting digestion: peptic secretion.
b. Induced by or associated with the action of digestive secretions: a peptic ulcer.
2. Of, relating to, or involving pepsin.
3. Capable of digesting.
n.
A digestive agent.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
pep·tic
(pep'tik)Relating to the stomach, to gastric digestion, or to pepsin A.
[G. peptikos, fr. peptō, to digest]
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
Peptic
Induced by or associated with the action of digestive secretions.
Mentioned in: H-2 Blockers
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
pep·tic
, pepsic (pep'tik, -sik)Relating to stomach, to gastric digestion, or to pepsin A.
[G. peptikos, fr. peptō, to digest]
Medical Dictionary for the Dental Professions © Farlex 2012
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp