Medical term:
polycyesis
pregnancy
[preg´nan-se]the condition of having a developing embryo or fetus in the body, after union of an oocyte (ovum) and spermatozoon. The average gestation period for a human pregnancy is 10 lunar months (280 days) from the first day of the last menstrual period.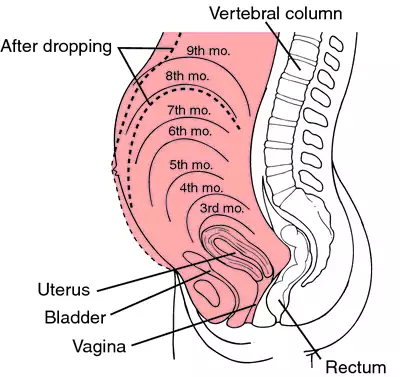
Conception. Once a month an ovum (secondary oocyte) matures in one of the ovaries and travels down the nearby fallopian tube to the uterus; this process is called ovulation. At Fertilization, which must take place within a day or two of ovulation, one of the spermatozoa unites with the ovum to form a zygote. The zygote then implants itself in the wall of the uterus, which is richly supplied with blood, and begins to grow. (See also reproduction.)
Signs of Pregnancy. Usually the first indication of pregnancy is a missed menstrual period. Unless the period is more than 10 days late, however, this is not a definite indication, since many factors, including a strong fear of pregnancy, can delay menstruation. Nausea, or morning sickness, usually begins in the fifth or sixth week of pregnancy. About 4 weeks after conception, changes in the breasts become noticeable: there may be a tingling sensation in the breasts, the nipples enlarge, and the areolae (dark areas around nipples) may become darker. Frequent urination, another early sign, is the result of expansion of the uterus, which presses on the bladder.
Other signs of pregnancy include softening of the cervix and filling of the cervical canal with a plug of mucus. Early in labor this plug is expelled and there is slight bleeding; expulsion of the mucous plug is known as show and indicates the beginning of cervical dilatation. chadwick's sign of pregnancy refers to a bluish color of the vagina which is a result of increased blood supply to the area.
When the abdominal wall becomes stretched there may be a breaking down of elastic tissues, resulting in depressed areas in the skin which are smooth and reddened. These markings are called striae gravidarum. In subsequent pregnancies the old striae appear as whitish streaks and frequently do not disappear completely.
There are several fairly accurate laboratory tests for pregnancy; all are designed to detect human chorionic gonadotropin (hCG), a hormone produced by living chorionic placental tissue and evident in the blood and urine of pregnant women. See also pregnancy tests.
Other signs of pregnancy include softening of the cervix and filling of the cervical canal with a plug of mucus. Early in labor this plug is expelled and there is slight bleeding; expulsion of the mucous plug is known as show and indicates the beginning of cervical dilatation. chadwick's sign of pregnancy refers to a bluish color of the vagina which is a result of increased blood supply to the area.
When the abdominal wall becomes stretched there may be a breaking down of elastic tissues, resulting in depressed areas in the skin which are smooth and reddened. These markings are called striae gravidarum. In subsequent pregnancies the old striae appear as whitish streaks and frequently do not disappear completely.
There are several fairly accurate laboratory tests for pregnancy; all are designed to detect human chorionic gonadotropin (hCG), a hormone produced by living chorionic placental tissue and evident in the blood and urine of pregnant women. See also pregnancy tests.
Growth of the Fetus. The average pregnancy lasts about 280 days, or 40 weeks, from the date of conception to childbirth. Since the exact date of conception usually is not known, the estimated date of delivery can be calculated using nägele's rule. This is approximate, since pregnancy may be shorter than the average or can last as long as 300 days. (For stages of growth of the fetus, see fetus.)
Care of the Fetus. A host of influences can adversely affect the growth and development of the fetus and his or her chances for survival and good health after birth. The diet of the mother should be nutritious and well-balanced so that the fetus receives the necessary food elements for development and maturity of body structures. It is especially important that the mother receive adequate protein in her diet, because a protein deficiency can hamper fetal intellectual development. Supplemental iron and vitamins usually are recommended during pregnancy.
There is now less emphasis on severe restriction of the mother's dietary intake to maintain a limited weight gain. The average gain is about 28 lb during pregnancy, and either starvation diets or forced feedings can be unhealthy for the mother and hazardous for the fetus. Ideally, the mother should achieve normal weight before she becomes pregnant because obesity increases the possibility of eclampsia and other serious complications of pregnancy. Mothers who are underweight are more likely to deliver immature babies who, by virtue of their physiologic immaturity, are more likely to suffer from birth defects, hyaline membrane disease, and other developmental disorders of the newborn.
Other factors affecting the fetus include certain drugs taken by the mother during pregnancy. A well-known example is thalidomide, which inhibits the growth of the extremities of the fetus, resulting in gross deformities. Many drugs, including prescription as well as nonprescription medications, are now believed to be capable of causing fetal abnormalities. In addition, consumption of alcohol during pregnancy may result in fetal alcohol syndrome. Most health care providers recommend that all drugs be avoided during pregnancy except those essential to the control of disease in the mother.
Diseases that increase the risk of obstetrical complications include diabetes, heart disease, hypertension, kidney disease, and anemia. rubella (German measles) can be responsible for many types of birth defects, particularly if the mother contracts it in the first 3 months of pregnancy. Sexually transmitted diseases can have tragic effects on the baby, even though the symptoms in the mother are minor at the time of pregnancy. syphilis is particularly dangerous because it is one of the few diseases that can be transmitted to the fetus in utero. The baby is either stillborn or born infected, and rarely escapes physical or mental defects or both. Successful treatment of the mother before the fifth month of pregnancy will prevent infection in the infant.
During the birth process the infant may be infected with gonorrhea as it passes through the birth canal. Gonorrheal infection of the eyes can cause blindness. herpes simplex Type II involving the genitals of the mother can also be transmitted to the infant at birth. The mortality and morbidity rates for such infected infants are high.
The age of the mother is also an important factor in the well-being of the fetus. The mortality and morbidity rate for infants born of mothers below age 15 and above 40 are higher than for those of mothers between these ages.
Recently developed tests to monitor fetal health have taken much of the guesswork out of predicting the chances of survival and health status of the fetus after birth. Such tests and evaluation techniques include amniocentesis, chemical and hormonal assays, biophysical profiles, testing for alpha-fetoprotein, ultrasound examinations, electronic surveillance of fetal vital signs and reaction to uterine contractions, and analyses of the infant's blood during labor.
There is now less emphasis on severe restriction of the mother's dietary intake to maintain a limited weight gain. The average gain is about 28 lb during pregnancy, and either starvation diets or forced feedings can be unhealthy for the mother and hazardous for the fetus. Ideally, the mother should achieve normal weight before she becomes pregnant because obesity increases the possibility of eclampsia and other serious complications of pregnancy. Mothers who are underweight are more likely to deliver immature babies who, by virtue of their physiologic immaturity, are more likely to suffer from birth defects, hyaline membrane disease, and other developmental disorders of the newborn.
Other factors affecting the fetus include certain drugs taken by the mother during pregnancy. A well-known example is thalidomide, which inhibits the growth of the extremities of the fetus, resulting in gross deformities. Many drugs, including prescription as well as nonprescription medications, are now believed to be capable of causing fetal abnormalities. In addition, consumption of alcohol during pregnancy may result in fetal alcohol syndrome. Most health care providers recommend that all drugs be avoided during pregnancy except those essential to the control of disease in the mother.
Diseases that increase the risk of obstetrical complications include diabetes, heart disease, hypertension, kidney disease, and anemia. rubella (German measles) can be responsible for many types of birth defects, particularly if the mother contracts it in the first 3 months of pregnancy. Sexually transmitted diseases can have tragic effects on the baby, even though the symptoms in the mother are minor at the time of pregnancy. syphilis is particularly dangerous because it is one of the few diseases that can be transmitted to the fetus in utero. The baby is either stillborn or born infected, and rarely escapes physical or mental defects or both. Successful treatment of the mother before the fifth month of pregnancy will prevent infection in the infant.
During the birth process the infant may be infected with gonorrhea as it passes through the birth canal. Gonorrheal infection of the eyes can cause blindness. herpes simplex Type II involving the genitals of the mother can also be transmitted to the infant at birth. The mortality and morbidity rates for such infected infants are high.
The age of the mother is also an important factor in the well-being of the fetus. The mortality and morbidity rate for infants born of mothers below age 15 and above 40 are higher than for those of mothers between these ages.
Recently developed tests to monitor fetal health have taken much of the guesswork out of predicting the chances of survival and health status of the fetus after birth. Such tests and evaluation techniques include amniocentesis, chemical and hormonal assays, biophysical profiles, testing for alpha-fetoprotein, ultrasound examinations, electronic surveillance of fetal vital signs and reaction to uterine contractions, and analyses of the infant's blood during labor.
Prenatal Care. The care of the mother during her entire pregnancy is important to her well-being and that of the fetus she is carrying. It will help provide ease and safety during pregnancy and childbirth. The health care provider learns about the patient's physical condition and medical history, and can detect possible complications before they become serious.
On the first prenatal visit the patient's medical history is taken in considerable detail, including any diseases or operations she has had, the course of previous pregnancies, if any, and whether there is a family history of multiple births or of diabetes mellitus or other chronic diseases. The first visit also includes a thorough physical examination and measurement of the pelvis. Blood samples are taken for screening for rubella and sexually transmitted diseases such as syphilis, hepatitis B, chlamydiosis, infection by the human immunodeficiency virus, and other conditions. A complete blood count is also needed. Urine is tested for albumin and sugar and examined microscopically. On subsequent visits the patient brings a urine specimen, collected upon arising that morning, to be tested for albumin and glucose. At each prenatal visit her blood pressure is taken and recorded and she is weighed. In the second trimester, when the uterus becomes an abdominal organ, the height of the fundus is measured at each visit. After the sixth month a rule such as mcdonald's rule can be applied to assess fetal growth.
Patients who are considered high-risk mothers usually are sent to a specialist and the infant is delivered at a regional hospital where sophisticated monitoring equipment and laboratory tests are available, and specially trained personnel can attend to the needs of the mother and her infant.
On the first prenatal visit the patient's medical history is taken in considerable detail, including any diseases or operations she has had, the course of previous pregnancies, if any, and whether there is a family history of multiple births or of diabetes mellitus or other chronic diseases. The first visit also includes a thorough physical examination and measurement of the pelvis. Blood samples are taken for screening for rubella and sexually transmitted diseases such as syphilis, hepatitis B, chlamydiosis, infection by the human immunodeficiency virus, and other conditions. A complete blood count is also needed. Urine is tested for albumin and sugar and examined microscopically. On subsequent visits the patient brings a urine specimen, collected upon arising that morning, to be tested for albumin and glucose. At each prenatal visit her blood pressure is taken and recorded and she is weighed. In the second trimester, when the uterus becomes an abdominal organ, the height of the fundus is measured at each visit. After the sixth month a rule such as mcdonald's rule can be applied to assess fetal growth.
Patients who are considered high-risk mothers usually are sent to a specialist and the infant is delivered at a regional hospital where sophisticated monitoring equipment and laboratory tests are available, and specially trained personnel can attend to the needs of the mother and her infant.
Discomforts and Complications.morning sickness usually appears in the early months of pregnancy and rarely lasts beyond the third month. Often it requires no treatment or can be relieved by such simple measures as eating dry crackers and tea before rising. Indigestion and heartburn are best prevented by avoiding foods that are difficult to digest, such as cucumbers, cabbage, cauliflower, spinach, onions, and rich foods. Constipation usually can be corrected by diet or a mild laxative; strong laxatives should not be used unless prescribed by the health care provider.
A visit to a dentist early in pregnancy is a good idea to forestall any possibility of infection arising from tooth decay. Pregnancy does not encourage tooth decay. Hemorrhoids sometimes occur in pregnancy because of pressure from the enlarged uterus on the veins in the rectum. The health care provider should be consulted for treatment. varicose veins also result from pressure of the uterus, which restricts the flow of blood from the legs and feet. Lying flat with the feet raised on a pillow several times a day will help relieve swelling and pain in the legs. In more difficult cases the health care provider may prescribe an elastic bandage or support stockings.
Backache during pregnancy is caused by the heavy abdomen pulling on muscles that are not normally used, and can be relieved by rest, sensible shoes, and good posture. Swelling of the feet and ankles usually is relieved by rest and by remaining off the feet for a day or two. If the swelling does not disappear, the health care provider should be informed since it may be an indication of a more serious complication.
Shortness of breath is common in the later stages of pregnancy. If at any time it becomes so extreme that the woman cannot climb a short flight of stairs without discomfort, the health care provider should be consulted. If a mild shortness of breath interferes with sleep, lying in a half-sitting position, supported by several pillows, may help.
The more serious complications of pregnancy include pyelitis, hyperemesis gravidarum, eclampsia, and placenta previa and abruptio placentae.
A visit to a dentist early in pregnancy is a good idea to forestall any possibility of infection arising from tooth decay. Pregnancy does not encourage tooth decay. Hemorrhoids sometimes occur in pregnancy because of pressure from the enlarged uterus on the veins in the rectum. The health care provider should be consulted for treatment. varicose veins also result from pressure of the uterus, which restricts the flow of blood from the legs and feet. Lying flat with the feet raised on a pillow several times a day will help relieve swelling and pain in the legs. In more difficult cases the health care provider may prescribe an elastic bandage or support stockings.
Backache during pregnancy is caused by the heavy abdomen pulling on muscles that are not normally used, and can be relieved by rest, sensible shoes, and good posture. Swelling of the feet and ankles usually is relieved by rest and by remaining off the feet for a day or two. If the swelling does not disappear, the health care provider should be informed since it may be an indication of a more serious complication.
Shortness of breath is common in the later stages of pregnancy. If at any time it becomes so extreme that the woman cannot climb a short flight of stairs without discomfort, the health care provider should be consulted. If a mild shortness of breath interferes with sleep, lying in a half-sitting position, supported by several pillows, may help.
The more serious complications of pregnancy include pyelitis, hyperemesis gravidarum, eclampsia, and placenta previa and abruptio placentae.
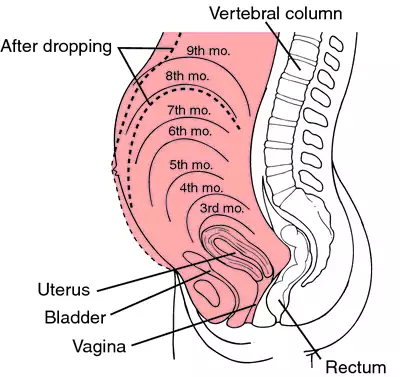
Uterine levels in pregnancy.
abdominal pregnancy ectopic pregnancy within the peritoneal cavity.
ampullar pregnancy ectopic pregnancy in the ampulla of the fallopian tube.
cervical pregnancy ectopic pregnancy within the cervical canal.
combined pregnancy simultaneous intrauterine and extrauterine pregnancies.
cornual pregnancy pregnancy in a horn of the uterus.
ectopic pregnancy pregnancy in which the fertilized ovum becomes implanted outside the uterus instead of in the wall of the uterus; this is almost always in a fallopian tube (tubal pregnancy), although occasionally the ovum develops in the abdominal cavity, ovary, or cervix uteri. Called also extrauterine pregnancy.
In a tubal pregnancy a spontaneous abortion may occur, but more often the fetus will grow to a size large enough to rupture the tube. This is an emergency situation requiring immediate treatment. The symptoms of such a tubal rupture are vaginal bleeding and severe pain in one side of the abdomen. Prompt surgery is necessary to remove the damaged tube and the fetus, and to stop the bleeding. Fortunately, the removal of one tube usually leaves the other one intact, so that future pregnancy is possible. Patients who are Rh-negative should be given Rh0 (D) immune globulin (RhoGAM) after ectopic pregnancy for isoimmunization protection in future pregnancies.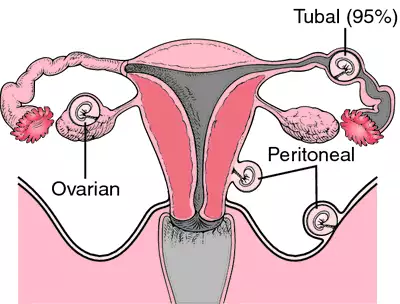
In a tubal pregnancy a spontaneous abortion may occur, but more often the fetus will grow to a size large enough to rupture the tube. This is an emergency situation requiring immediate treatment. The symptoms of such a tubal rupture are vaginal bleeding and severe pain in one side of the abdomen. Prompt surgery is necessary to remove the damaged tube and the fetus, and to stop the bleeding. Fortunately, the removal of one tube usually leaves the other one intact, so that future pregnancy is possible. Patients who are Rh-negative should be given Rh0 (D) immune globulin (RhoGAM) after ectopic pregnancy for isoimmunization protection in future pregnancies.
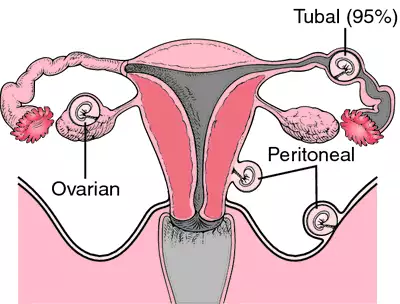
Ectopic pregnancy. The fallopian tube is the most common site for ectopic pregnancies but they can also occur on the ovary or the peritoneal surface of the abdominal cavity. From Damjanov, 2000.
extrauterine pregnancy ectopic pregnancy.
false pregnancy development of all the signs of pregnancy without the presence of an embryo; called also pseudocyesis and pseudopregnancy.
interstitial pregnancy pregnancy in that part of the fallopian tube within the wall of the uterus.
intraligamentary pregnancy (intraligamentous pregnancy) ectopic pregnancy within the broad ligament.
molar pregnancy conversion of the fertilized ovum into a mole.
multiple pregnancy the presence of more than one fetus in the uterus at the same time.
mural pregnancy interstitial pregnancy.
ovarian pregnancy pregnancy occurring in an ovary.
phantom pregnancy false pregnancy due to psychogenic factors.
surrogate pregnancy one in which a woman other than the female partner is artificially impregnated with the male partner's sperm. The resultant child represents only the male of the marital unit, and may be adopted by the female.
pregnancy tests procedures for early determination of pregnancy. By the first missed menstrual period or shortly thereafter, human chorionic gonadotropin (hCG), a hormone secreted by the placenta, is present in the blood and urine of a pregnant woman. It was formerly determined by bioassay in which a urine or serum specimen was injected into a laboratory animal and the response of ovarian tissue was noted. All testing now uses immunologic techniques based on antigen-antibody binding between hCG and anti-hCG antibody. There are several commercial kits available (see early pregnancy tests), based on the agglutination of hCG-coated latex particles by anti-hCG serum, which is inhibited if the urine specimen added to the serum contains hCG. Clinical laboratories generally use radioimmunoassay or radioreceptor assay to determine serum hCG levels. These methods are more accurate and less likely to produce false-positive results.
tubal pregnancy the most common type of ectopic pregnancy, occurring within a fallopian tube.
tuboabdominal pregnancy ectopic pregnancy occurring partly in the fimbriated end of the fallopian tube and partly in the abdominal cavity.
tubo-ovarian pregnancy pregnancy at the fimbriae of the fallopian tube.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
mul·ti·ple preg·nan·cy
condition of bearing two or more fetuses simultaneously.
Synonym(s): polycyesis
Farlex Partner Medical Dictionary © Farlex 2012
mul·ti·ple preg·nan·cy
(mŭl'ti-pĕl preg'năn-sē)Condition of bearing two or more fetuses simultaneously.
Synonym(s): polycyesis.
Synonym(s): polycyesis.
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
Latest Searches:
Voraxaze - Voranil - Voorhoeve - voodoo - VOO - Vontrol - von - vomitus - vomiturition - vomitory - vomitoria - vomito - vomitive - vomiting - vomit - vomica - vomerovaginalis - vomerovaginal - vomerorostralis - vomerorostral -
- Service manuals - MBI Corp